Korean Diabetes J.
2008 Dec;32(6):467-473. 10.4093/kdj.2008.32.6.467.
Mitochondrial Dysfunction in Diabetic Cardiomyopathy
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Chung-Ang University College of Medicine, Korea.
- KMID: 2222453
- DOI: http://doi.org/10.4093/kdj.2008.32.6.467
Abstract
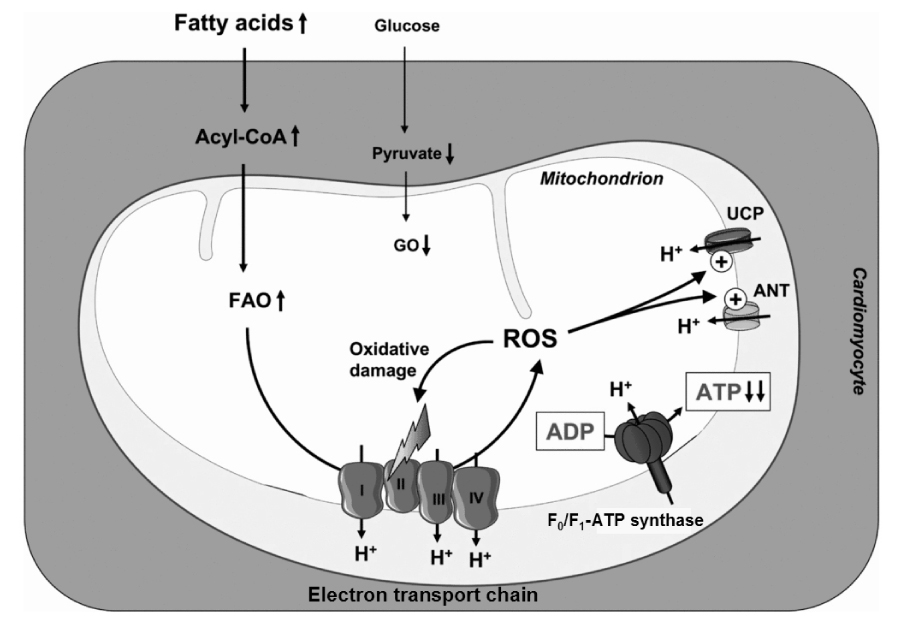
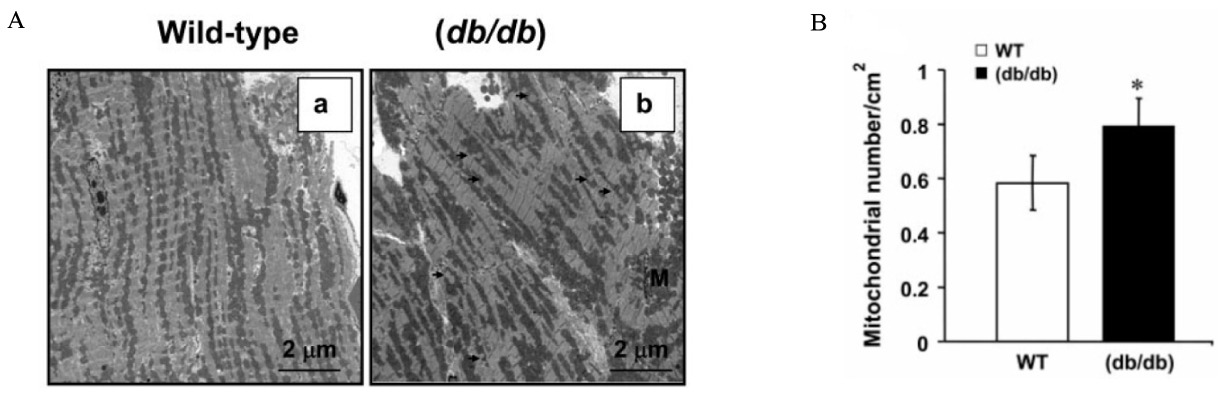
- Metabolic syndrome and diabetes are associated with increased risk of cardiac dysfunction independently of underlying coronary artery disease. The underlying pathogenesis is partially understood but accumulating evidence suggests that alterations of cardiac energy metabolism might contribute to the development of contractile dysfunction. Recent findings suggest that myocardial mitochondrial dysfunction may play an important role in the pathogenesis of cardiac contractile dysfunction in type 2 diabetes. This review is focused on evaluating mechanisms for the mitochondrial abnormalities that may be involved in the development and progression of cardiac dysfunction in diabetes.
Keyword
Figure
Reference
-
1. Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979. 241:2035–2038.
Article2. Rubler S, Dlugash J, Yuceoglu YZ, Kumral T, Branwood AW, Grishman A. New type of cardiomyopathy associated with diabetic glomerulo- sclerosis. Am J Cardiol. 1972. 30:595–602.3. Boudina S, Abel ED. Diabetic cardiomyopathy revisited. Circulation. 2007. 115:3213–3223.
Article4. Borezuk A, Factor SM. Chatham JC, Forder JR, McNeill JH, editors. Pathological alterations of the heart in diabetes mellitus. The heart in diabetes. 1996. Norwell, MA: Kluwer Academic Publishers;23–40.5. Asbun J, Villarreal FJ. The pathogenesis of myocardial fibrosis in the setting of diabetic cardiomyopathy. J Am Coll Cardiol. 2006. 47:693–700.
Article6. Buchanan J, Mazumder PK, Hu P, Chakrabarti G, Roberts MW, Yun UJ, Cooksey RC, Litwin SE, Abel ED. Reduced cardiac efficiency and altered substrate metabolism precedes the onset of hyperglycemia and contractile dysfunction in two mouse models of insulin resistance and obesity. Endocrinology. 2005. 146:5341–5349.
Article7. Mazumder PK, O'Neill BT, Roberts MW, Buchanan J, Yun UJ, Cooksey RC, Boudina S, Abel ED. Impaired cardiac efficiency and increased fatty acid oxidation in insulin-resistant ob/ob mouse hearts. Diabetes. 2004. 53:2366–2374.
Article8. McGavock JM, Victor RG, Unger RH, Szczepaniak LS. Adiposity of the heart, revisited. Ann Intern Med. 2006. 144:517–524.
Article9. Sharma S, Adrogue JV, Golfman L, Uray I, Lemm J, Youker K, Noon GP, Frazier OH, Taegtmeyer H. Intramyocardial lipid accumulation in the failing human heart resembles the lipotoxic rat heart. FASEB J. 2004. 18:1692–1700.
Article10. Szczepaniak LS, Dobbins RL, Metzger GJ, Sartoni-D'Ambrosia G, Arbique D, Vongpatanasin W, Unger R, Victor RG. Myocardial triglycerides and systolic function in humans: in vivo evaluation by localized proton spectroscopy and cardiac imaging. Magn Reson Med. 2003. 49:417–423.
Article11. Yang J, Sambandam N, Han X, Gross RW, Courtois M, Kovacs A, Febbraio M, Finck BN, Kelly DP. CD36 deficiency rescues lipotoxic cardiomyopathy. Circ Res. 2007. 100:1208–1217.
Article12. Finck BN, Lehman JJ, Leone TC, Welch MJ, Bennett MJ, Kovacs A, Han X, Gross RW, Kozak R, Lopaschuk GD, Kelly DP. The cardiac phenotype induced by PPARalpha overexpression mimics that caused by diabetes mellitus. J Clin Invest. 2002. 109:121–130.13. Finck BN, Han X, Courtois M, Aimond F, Nerbonne JM, Kovacs A, Gross RW, Kelly DP. A critical role for PPARalpha-mediated lipotoxicity in the pathogenesis of diabetic cardiomyopathy: modulation by dietary fat content. Proc Natl Acad Sci U S A. 2003. 100:1226–1231.14. Finck BN. The role of the peroxisome proliferator-activated receptor alpha pathway in pathological remodeling of the diabetic heart. Curr Opin Clin Nutr Metab Care. 2004. 7:391–396.
Article15. Aoyama T, Peters JM, Iritani N, Nakajima T, Furihata K, Hashimoto T, Gonzalez FJ. Altered constitutive expression of fatty acid-metabolizing enzymes in mice lacking the peroxisome proliferator-activated receptor alpha. J Biol Chem. 1998. 273:5678–5684.16. Lee SS, Pineau T, Drago J, Lee EJ, Owens JW, Kroetz DL, Fernandez-Salguero PM, Westphal H, Gonzalez FJ. Targeted disruption of the alpha isoform of the peroxisome proliferator-activated receptor gene in mice results in abolishment of the pleiotropic effects of peroxisome proliferators. Mol Cell Biol. 1995. 15:3012–3022.
Article17. Dagenais GR, Jalbert B. Effect of increased free fatty acids on myocardial oxygen extraction and angina threshold during atrial pacing. Circulation. 1977. 56:315–319.
Article18. Pearce FJ, Forster J, DeLeeuw G, Williamson JR, Tutwiler GF. Inhibition of fatty acid oxidation and in normal and hypoxic perfused rat hearts by 2-tetradecylglycidic acid. J Mol Cell Cardio. 1979. 11:893–915.19. Vik-Mo H, Mjos OD. Influence of free fatty acids on myocardial oxygen consumption and ischemic injury. Am J Cardiol. 1981. 48:361–365.
Article20. An D, Rodrigues B. Role of changes in cardiac metabolism in development of diabetic cardiomyopathy. Am J Physiol Heart Circ Physiol. 2006. 291:H1489–H1506.
Article21. Herrero P, Peterson LR, McGill JB, Matthew S, Lesniak D, Dence C, Gropler RJ. Increased myocardial fatty acid metabolism in patients with type 1 diabetes mellitus. J Am Coll Cardiol. 2006. 47:598–604.
Article22. Peterson LR, Herrero P, McGill J, Schechtman KB, Kisrieva-Ware Z, Lesniak D, Gropler RJ. Fatty acids and insulin modulate myocardial substrate metabolism in humans with type 1 diabetes. Diabetes. 2008. 57:32–40.
Article23. Hafstad AD, Khalid AM, How OJ, Larsen TS, Aasum E. Glucose and insulin improve cardiac efficiency and post-ischemic functional recovery in perfused hearts from type 2 diabetic (db/db) mice. Am J Physiol Endocrinol Metab. 2007. 292:E1288–E1294.
Article24. Ledesma A, de Lacoba MG, Rial E. The mitochondrial uncoupling proteins. Genome Biol. 2002. 3:REVIEWS3015.25. Nicholls DG, Locke RM. Thermogenic mechanisms in brown fat. Physiol Rev. 1984. 64:1–64.
Article26. Boss O, Samec S, Paoloni-Giacobino A, Rossier C, Dulloo A, Seydoux J, Muzzin P, Giacobino JP. Uncoupling protein-3: a new member of the mitochondrial carrier family with tissue-specific expression. FEBS Lett. 1997. 408:39–42.
Article27. Gong DW, He Y, Karas M, Reitman M. Uncoupling protein-3 is a mediator of thermogenesis regulated by thyroid hormone, beta3-adrenergic agonists, and leptin. J Biol Chem. 1997. 272:24129–24132.28. Brand MD, Esteves TC. Physiological functions of the mitochondrial uncoupling proteins UCP2 and UCP3. Cell Metab. 2005. 2:85–93.
Article29. Lambert AJ, Brand MD. Superoxide production by NADH:ubiquinone oxidoreductase (complex I) depends on the pH gradient across the mitochondrial inner membrane. Biochem J. 2004. 382:511–517.
Article30. Nishikawa T, Edelstein D, Du XL, Yamagishi S, Matsumura T, Kaneda Y, Yorek MA, Beebe D, Oates PJ, Hammes HP, Giardino I, Brownlee M. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature. 2000. 404:787–790.
Article31. Young ME, Patil S, Ying J, Depre C, Ahuja HS, Shipley GL, Stepkowski SM, Davies PJ, Taegtmeyer H. Uncoupling protein 3 transcription is regulated by peroxisome proliferator-activated receptor in the adult rodent heart. FASEB J. 2001. 15:833–845.32. Chou CJ, Cha MC, Jung DW, Boozer CN, Hashim SA, Pi-Sunyer FX. High-fat diet feeding elevates skeletal muscle uncoupling protein 3 levels but not its activity in rats. Obes Res. 2001. 9:313–319.
Article33. Kageyama H, Suga A, Kashiba M, Oka J, Osaka T, Kashiwa T, Hirano T, Nemoto K, Namba Y, Ricquier D, Giacobino JP, Inoue S. Increased uncoupling protein-2 and -3 gene expressions in skeletal muscle of STZ-induced diabetic rats. FEBS Lett. 1998. 440:450–453.
Article34. Murray AJ, Anderson RE, Watson GC, Radda GK, Clarke K. Uncoupling proteins in human heart. Lancet. 2004. 364:1786–1788.
Article35. Ho OJ, Aasum E, Severson DL, Chan WY, Essop MF, Larsen TS. Increased myocardial oxygen consumption reduces cardiac efficiency in diabetic mice. Diabetes. 2006. 55:466–473.
Article36. Essop MF, Razeghi P, McLeod C, Young ME, Taegtmeyer H, Sack MN. Hypoxia-induced decrease of UCP3 gene expression in rat heart parallels metabolic gene switching but fails to affect mitochondrial respiratory coupling. Biochem Biophys Res Commun. 2004. 314:561–564.
Article37. Boudina S, Sena S, Theobald H, Sheng X, Wright JJ, Hu XX, Aziz S, Johnson JI, Bugger H, Zaha VG, Abel ED. Mitochondrial energetics in the heart in obesity related diabetes: direct evidence for increased uncoupled respiration and activation of uncoupling proteins. Diabetes. 2007. 56:2457–2466.38. Boudina S, Sena S, O'Neill BT, Tathireddy P, Young ME, Abel ED. Reduced mitochondrial oxidative capacity and increased mitochondrial uncoupling impair myocardial energetics in obesity. Circulation. 2005. 112:2686–2695.
Article39. Shen X, Zheng S, Thongboonkerd V, Xu M, Pierce WM Jr, Klein JB, Epstein PN. Cardiac mitochondrial damage and biogenesis in a chronic model of type 1 diabetes. Am J Physiol Endocrinol Meta. 2004. 287:E896–E905.
Article40. Finck BN, Kelly DP. Peroxisome proliferator-activated receptor gamma coactivator-1 (PGC-1) regulatory cascade in cardiac physiology and disease. Circulation. 2007. 115:2540–2548.41. Ventura-Clapier R, Garnier A, Veksler V. Transcriptional control of mitochondrial biogenesis: the central role of PGC-1alpha. Cardiovasc Res. 2008. 79:208–217.42. Duncan JG, Fong JL, Medeiros DM, Finck BN, Kelly DP. Insulin-resistant heart exhibits a mitochondrial biogenic response driven by the peroxisome proliferator-activated receptor/PGC-1 gene regulatory pathway. Circulation. 2007. 115:909–917.
Article43. Boudina S, Abel ED. Mitochondrial uncoupling: a key contributor to reduced cardiac efficiency in diabetes. Physiology (Bethesda). 2005. 21:250–258.
Article44. Bugger H, Abel ED. Molecular mechanisms for myocardial mitochondrial dysfunction in the metabolic syndrome. Clin Sci (Lond). 2008. 114:195–210.
Article