J Korean Ophthalmol Soc.
2012 Jul;53(7):953-959. 10.3341/jkos.2012.53.7.953.
Quantitative Measurement of Glare Disability Using a Glaremeter
- Affiliations
-
- 1Department of Ophthalmology and Institute of Vision Research, Yonsei University College of Medicine, Seoul, Korea. shadik@yuhs.ac
- 2ALC Ophthalmology Clinic, Seoul, Korea.
- KMID: 2215853
- DOI: http://doi.org/10.3341/jkos.2012.53.7.953
Abstract
- PURPOSE
To report glare disability measured by a glaremeter.
METHODS
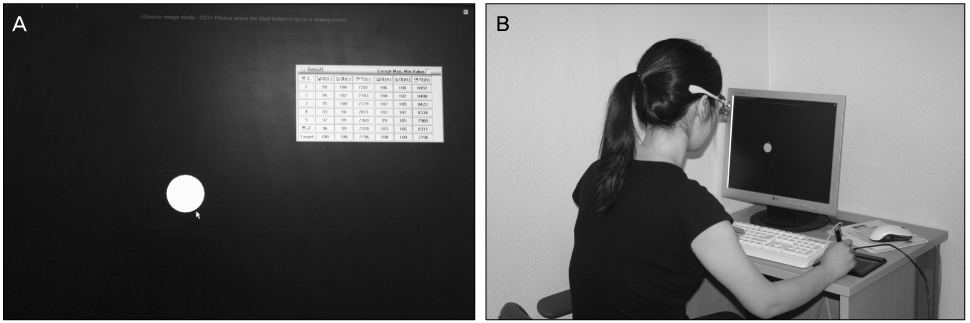
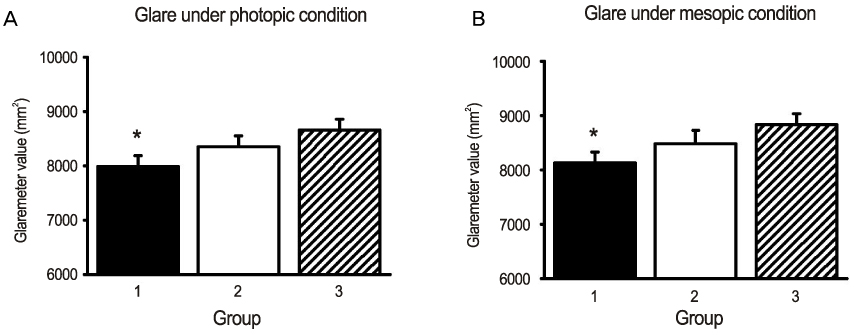
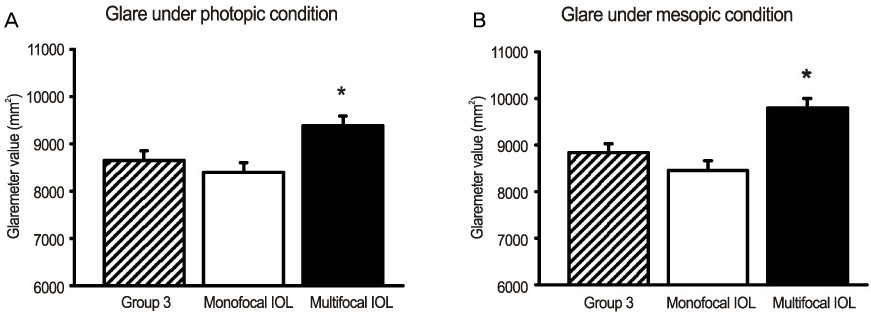
Glaremeter values were measured in 270 normal eyes and 100 pseudophakic eyes. The normal eyes were classified into 3 age groups (teenage to 60's) with 90 eyes in each group. The pseudophakic eyes were classified into the monofocal IOL (intraocular lens) and multifocal IOL implanted groups with 50 eyes in each group. Glaremeter values of each group were measured using a glaremeter under photopic (82.2 +/- 5.1 cd/m2) and mesopic (5.5 +/- 0.3 cd/m2) conditions.
RESULTS
The highest mean glaremeter value in the normal eyes was 8657.34 +/- 691.04 mm2 under the photopic condition and 8837.97 +/- 805.83 mm2 under the mesopic condition in the oldest group. The glaremeter value of the multifocal IOL implanted group was 9390.87 +/- 846.7 mm2 under the photopic condition and 9799.87 +/- 823.72 mm2 under the mesopic condition, which was significantly higher than the normal eye and the monofocal IOL implanted groups (p < 0.05).
CONCLUSIONS
In the normal population, the mean glaremeter values were increased according to age, and a significant increase was observed in the multifocal IOL implanted group. The present study results provide good basic data for cataract and presbyopia refractive surgery predicted to produce glare disability inevitably.
Keyword
Figure
Reference
-
1. Packer M, Fine IH, Hoffman RS. Functional vision, contrast sensitivity, and optical aberrations. Int Ophthalmol Clin. 2003. 43:1–3.2. Verdon W, Bullimore M, Maloney RK. Visual performance after photorefractive keratectomy. A prospective study. Arch Ophthalmol. 1996. 114:1465–1472.3. Ginsburg AP. Contrast sensitivity and functional vision. Int Ophthalmol Clin. 2003. 43:5–15.4. Ginsburg AP, Waring GO 3rd, Steinberg EB, et al. Contrast sensitivity under photopic conditions in the Prospective Evaluation of Radial Keratotomy (PERK) Study. Refract Corneal Surg. 1990. 6:82–91.5. Ghaith AA, Daniel J, Stulting RD, et al. Contrast sensitivity and glare disability after radial keratotomy and photorefractive keratectomy. Arch Ophthalmol. 1998. 116:12–18.6. Visser N, Nuijts RM, de Vries NE, Bauer NJ. Visual outcomes and patient satisfaction after cataract surgery with toric multifocal intraocular lens implantation. J Cataract Refract Surg. 2011. 37:2034–2042.7. Mutyala S, McDonald MB, Scheinblum KA, et al. Contrast sensitivity evaluation after laser in situ keratomileusis. Ophthalmology. 2000. 107:1864–1867.8. You YC, Choi TH, Lee HB. Normal contrast sensitivity for various ages. J Korean Ophthalmol Soc. 2003. 44:150–156.9. Ross JE, Bron AJ, Clarke DD. Contrast sensitivity and visual disability in chronic simple glaucoma. Br J Ophthalmol. 1984. 68:821–827.10. Regan D, Silver R, Murray TJ. Visual acuity and contrast sensitivity in multiple sclerosis--hidden visual loss: an auxiliary-diagnostic test. Brain. 1977. 100:563–579.11. Sen HN, Sarikkola AU, Uusitalo RJ, Laatikainen L. Quality of vision after AMO Array multifocal intraocular lens implantation. J Cataract Refract Surg. 2004. 30:2483–2493.12. Altaie R, Ring CP, Morarji J, et al. Prospective analysis of visual outcomes using apodized, diffractive multifocal intraocular lenses following phacoemulsification for cataract or clear lens extraction. Clin Experiment Ophthalmol. 2012. 40:148–154.13. Cheon MH, Lee JE, Kim JH, et al. One-year outcome of monocular implant of aspheric multifocal IOL. J Korean Ophthalmol Soc. 2010. 51:822–828.14. Kim SK, Kim JH, Kim EK, et al. Long-term quality of life after myopic laser refractive surgery. J Korean Ophthalmol Soc. 2011. 52:922–929.15. Lee HK, Choe CM, Ma KT, Kim EK. Measurement of contrast sensitivity and glare under mesopic and photopic conditions following wavefront-guided and conventional LASIK surgery. J Refract Surg. 2006. 22:647–655.16. van den Berg TJ. On the relation between glare and straylight. Doc Ophthalmol. 1991. 78:177–181.17. Coppens JE, Franssen L, van Rijn LJ, van den Berg TJ. Reliability of the compensation comparison stray-light measurement method. J Biomed Opt. 2006. 11:34027.18. Stifter E, Sacu S, Weghaupt H. Functional vision with cataracts of different morphologies: comparative study. J Cataract Refract Surg. 2004. 30:1883–1891.19. van Rijn LJ, Nischler C, Gamer D, et al. Measurement of stray light and glare: comparison of Nyktotest, Mesotest, stray light meter, and computer implemented stray light meter. Br J Ophthalmol. 2005. 89:345–351.20. Stifter E, Sacu S, Thaler A, Weghaupt H. Contrast acuity in cataracts of different morphology and association to self-reported visual function. Invest Ophthalmol Vis Sci. 2006. 47:5412–5422.21. Aslam TM, Haider D, Murray IJ. Principles of disability glare measurement: an ophthalmological perspective. Acta Ophthalmol Scand. 2007. 85:354–360.22. Lee SY, Oh JH. Straylight in normal and cataractous eyes of Koreans. J Korean Ophthalmol Soc. 2011. 52:182–189.23. Van Den Berg TJ, Van Rijn LJ, Michael R, et al. Straylight effects with aging and lens extraction. Am J Ophthalmol. 2007. 144:358–363.24. Chiam PJ, Chan JH, Aggarwal RK, Kasaby S. ReSTOR intraocular lens implantation in cataract surgery: quality of vision. J Cataract Refract Surg. 2006. 32:1459–1463.25. Lee HS, Park SH, Kim MS. Clinical results and some problems of multifocal apodized diffractive intraocular lens implantation. J Korean Ophthalmol Soc. 2008. 49:1235–1241.26. McCarty CA, Keeffe JE, Taylor HR. The need for cataract surgery: projections based on lens opacity, visual acuity, and personal concern. Br J Ophthalmol. 1999. 83:62–65.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study of Mesopic Vision and Glare in Normal Subjects and Post-LASIK Patients Using Mesoptometer
- Assessment of Posterior Capsular Opacification of Korean Using Straylight and Glare Sensitivity Meter
- The Aasesament of Contrast Sensitivity by MCT 8000(R) in Normal Eyes and Peeudophakic Eyes
- Two Cases of Glare after Iridotomy for Phakic Intraocular Lens Implantation
- A Study on the Usefulness of the AAPM TG18 Evaluation Tool for Diagnostic Monitor QC