J Korean Ophthalmol Soc.
2007 Oct;48(10):1303-1311. 10.3341/jkos.2007.48.10.1303.
Changes in Eyelid Height with Time after Levator Resection under Local Anesthesia
- Affiliations
-
- 1Happy Eye Clinic, Seoul, Korea.
- 2Department of Ophthalmology, Samsung Medical Center, School of Medicine Sungkyunkwan University, Seoul, Korea. ydkim@smc.samsung.co.kr
- KMID: 2210981
- DOI: http://doi.org/10.3341/jkos.2007.48.10.1303
Abstract
-
PURPOSE: To evaluate the factors that affect the eyelid height changes during the postoperative period in patients who underwent levator resection under local anesthesia.
METHODS
Among the 242 patients that underwent levator resection under local anesthesia by the same surgeon between January on 1995 and December 2003, marginal reflex distance 1 (MRD1) measurements were performed using a caliper in 91 patients who were followed for more than 3 months.
RESULTS
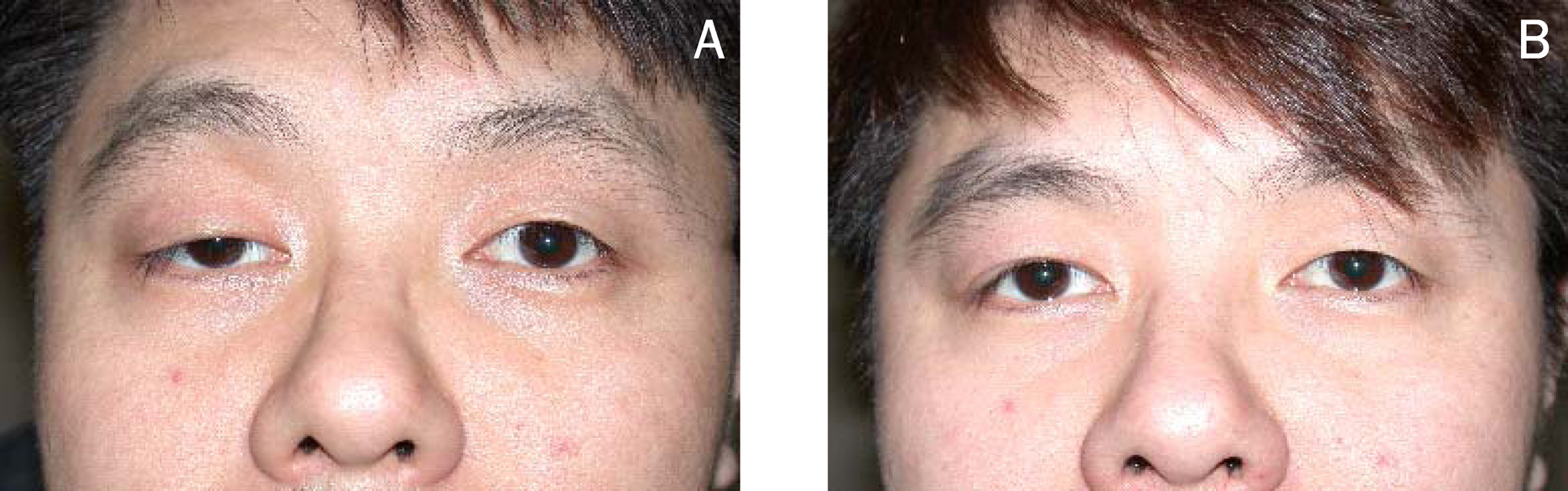
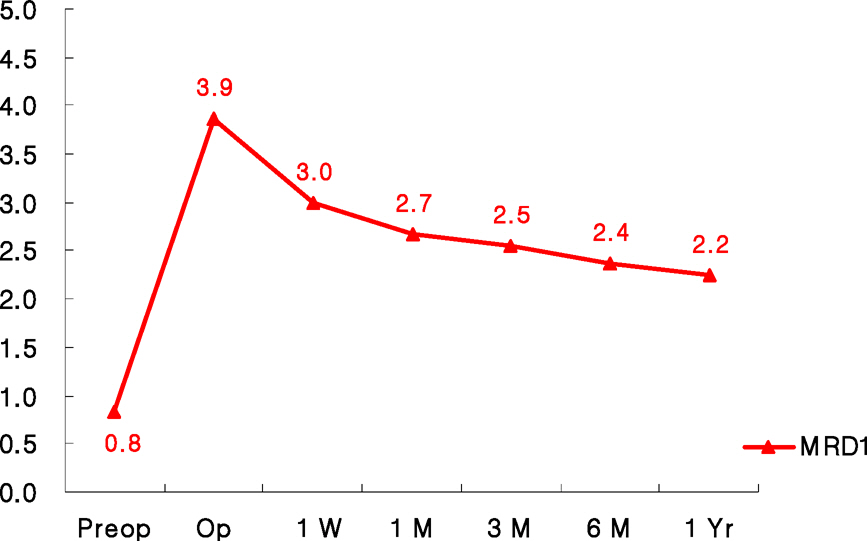
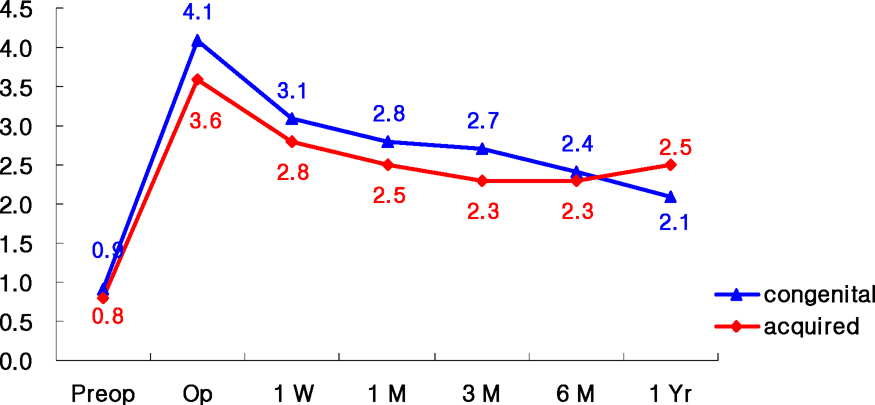
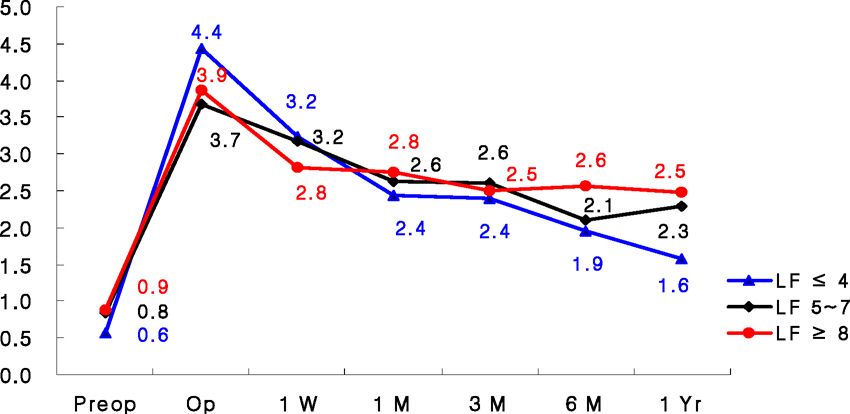
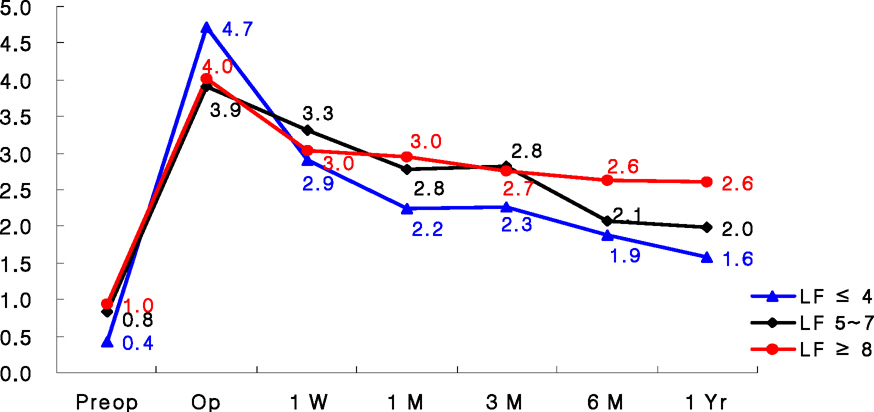
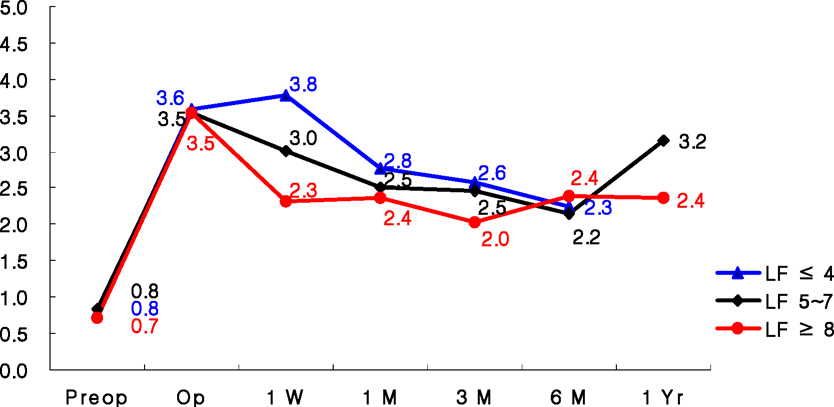
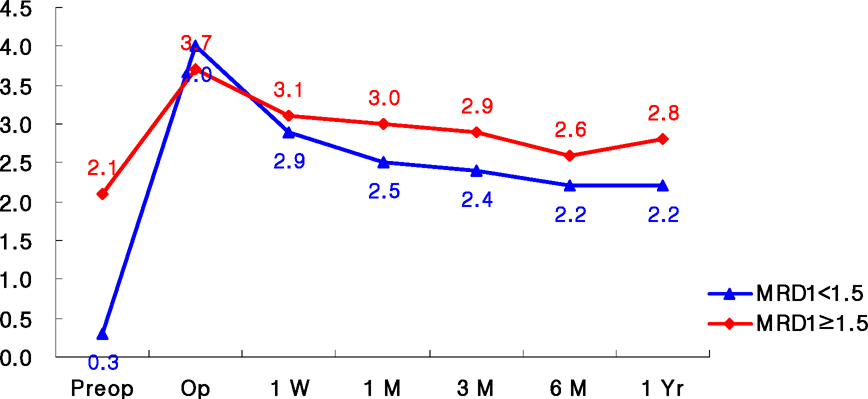
There were 36 males and 55 females, aged between 12 and 78 years (average of 33.6 years). The average follow-up period of the patients was 8.7 months (3 months ~ 58 months). During this period, 86 patients (94.5%) experienced satisfactory results. The average change in the MRD1 of the eyelids preoperatively, during the operation, and 1 week, 1 month, 3 months, 6 months, and 1 year postoperatively were 0.8 mm, 3.9 mm, 3.0 mm, 2.7 mm, 2.5 mm, 2.4 mm, and 2.2 mm, respectively. The MRD1 decreased 1.2 mm after 1 month and stabilized. When the levator function was greater than 8 mm, the height of the eyelids stabilized within 1 week. The worse the function of the levator palpebrae, such as in the case of congenital ptosis, the greater the correction was needed.
CONCLUSIONS
Levator resection under local anesthesia is a preferable method in adjusting the height of the eyelids. In a patient with poor levator function, a greater amount of correction is needed to achieve a satisfactory eyelid height.
Keyword
Figure
Cited by 2 articles
-
The Preference of Lid Height and Laterality with an Ocular Prosthesis in Korean Patients
Hyun Uk Shin, Long Yu Jin, Ji Young Suh, Hee Bae Ahn
J Korean Ophthalmol Soc. 2019;60(4):308-314. doi: 10.3341/jkos.2019.60.4.308.Surgical Outcomes of Levator Resection in Ptosis Patients with Deep Superior Sulcus
Jong Soo Kim, Hee Bae Ahn
J Korean Ophthalmol Soc. 2014;55(12):1734-1738. doi: 10.3341/jkos.2014.55.12.1734.
Reference
-
References
1. Anderson RL, Dixon RS. Aponeurotic ptosis surgery. Arch Ophthalmol. 1979; 97:1123–8.
Article2. Older JJ. Levator aponeurosis surgery for the correction of acquired ptosis : analysis of 113 procedures. Ophthalmology. 1983; 90:1056–9.3. Lee JY. A statistical study on the corneal diameters in Korean. J Korean Ophthalmol Soc. 1983; 24:53–8.4. Linberg JV, Vasquez RJ, Chao GM. Aponeurotic ptosis repair under local anesthesia : prediction of results from operative lid height. Ophthalmology. 1988; 95:1046–52.5. Crawford JS. Frontalis sling operation. J Pediatr Ophthalmol Strabismus. 1982; 19:253–5.
Article6. Lee KY, Chi YH, Woo KI, Kim YD. Frontalis sling operation using preserved fascia lata. J Korean Ophthalmol Soc. 1997; 38:2084–90.7. Chung PJ, Chung WS. Aponeurotic ptosis surgery. J Korean Ophthalmol Soc. 1990; 31:255–63.8. Mauriello JA, Wagner RS, Caputo AR, et al. Treatment of congenital ptosis by maximal levator resection. Ophthalmology. 1985; 93:466–9.
Article9. Fasanella RM, Servat J. Levator resection for minimal ptosis : another simplified operation. Arch Ophthalmol. 1961; 65:493–6.10. Choe KS, Kim YS, Lee TS. A clinical study of surgical results on 456 blepharoptosis. J Korean Ophthalmol Soc. 1995; 36:1093–104.11. Anderson RL, Beard C. The levator aponeurosis : Attachments and their clinical significance. Arch Ophthalmol. 1977; 95:1437–41.12. Jones LT. The anatomy of the upper eyelid and its relation to ptosis surgery. Am J Ophthamol. 1964; 57:943–59.
Article13. Kim YD, Shin KS. Surgical correction of acquired ptosis due to an aponeurotic defect. J Korean Ophthalmol Soc. 1990; 31:837–44.14. Linberg JV, Vasquez RJ, Chao GM. Aponeurotic ptosis repair under local anesthesia : prediction of results from operative lid height. Ophthalmology. 1988; 95:1046–52.15. Yang HS, Ahn JH, Kim SJ, Han YS. Surgical results of levator resection using the MLD in congenital blepharoptosis. J Korean Ophthalmol Soc. 2000; 41:2247–53.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Eyelid Blink Characteristics in Patients with Ptosis Assessed Using Cellphone Camera before and after Levator Resection
- Eyelid Stretching Exercise Performed in Overcorrection after Levator Resection in Congenital Ptosis
- Double Fold Affected by Levator Function in Simultaneous Double Eyelid Blepharoplasty with Blepharoptosis Surgery
- Double eyelid operation in blepharoptosis patients
- TREATMENT OF MARCUS GUNN PHENOMENON