Blood Res.
2013 Dec;48(4):254-257. 10.5045/br.2013.48.4.254.
Clinical characteristics of hemophagocytic lymphohistiocytosis following Kawasaki disease: differentiation from recurrent Kawasaki disease
- Affiliations
-
- 1Department of Pediatrics, Hanyang University College of Medicine, Seoul, Korea. cord@hanyang.ac.kr
- 2Department of Pediatrics, Ewha Womans University School of Medicine, Seoul, Korea.
- 3Department of Pediatrics, Keimyung University, Dongsan Medical Center, Daegu, Korea.
- 4Department of Pediatrics, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 2172872
- DOI: http://doi.org/10.5045/br.2013.48.4.254
Abstract
- BACKGROUND
Our aim was to investigate the clinical pattern of hemophagocytic lymphohistiocytosis following Kawasaki disease (HLH-KD), to enable differentiation of HLH from recurrent or refractory KD and facilitate early diagnosis.
METHODS
We performed a nationwide retrospective survey and reviewed the clinical characteristics of patients with HLH-KD, including the interval between KD and HLH, clinical and laboratory findings, treatment responses, and outcomes, and compared them with historical data for both diseases.
RESULTS
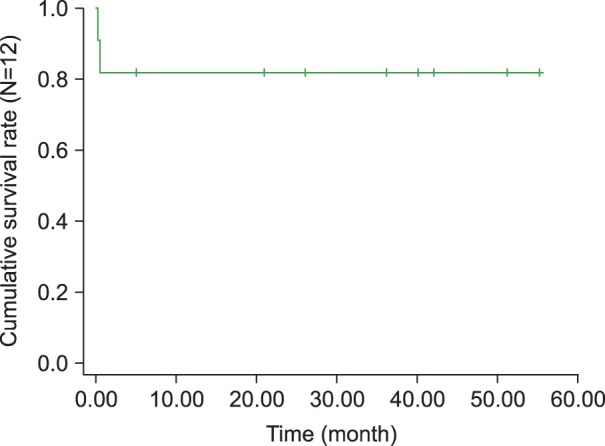
Twelve patients with HLH-KD, including 5 previously reported cases, were recruited. The median age was 6.5 years (range, 9 months-14.7 years). Eight patients were male and 4 were female. The median interval between the first episode of KD and the second visit with recurrent fever was 12 days (3-22 days). Of the 12 children, 2 were initially treated with intravenous IgG (IVIG) for recurrent KD when they presented at the hospital with recurrent fever. Eventually, 10 children received chemotherapy under an HLH protocol and 2 received supportive treatment. Two patients died of combined infections during chemotherapy, 1 was lost to follow up, and 9 remain alive. The overall survival rate at 4 years was 81.1% with a median follow up of 45.1 months.
CONCLUSION
A diagnosis of HLH-KD should be considered when symptoms similar to recurrent KD develop within 1 month of the first episode of KD. Our findings will help physicians differentiate between HLH and the recurrent form of KD.
MeSH Terms
Figure
Reference
-
1. Palazzi D, McClain K, Kaplan S. Hemophagocytic syndrome after Kawasaki disease. Pediatr Infect Dis J. 2003; 22:663–666. PMID: 12886898.
Article2. Grom A. Macrophage activation syndrome and reactive hemophagocytic lymphohistiocytosis: the same entities? Curr Opin Rheumatol. 2003; 15:587–590. PMID: 12960485.
Article3. Ravelli A. Macrophage activation syndrome. Curr Opin Rheumatol. 2002; 14:548–552. PMID: 12192253.
Article4. Sawhney S, Woo P, Murray KJ. Macrophage activation syndrome: a potentially fatal complication of rheumatic disorders. Arch Dis Child. 2001; 85:421–426. PMID: 11668110.
Article5. Muise A, Tallett SE, Silverman ED. Are children with Kawasaki disease and prolonged fever at risk for macrophage activation syndrome? Pediatrics. 2003; 112:e495. PMID: 14654653.
Article6. Al-Eid W, Al-Jefri A, Bahabri S, Al-Mayouf S. Hemophagocytosis complicating Kawasaki disease. Pediatr Hematol Oncol. 2000; 17:323–329. PMID: 10845231.
Article7. Kaneko K, Takahashi K, Fujiwara S, Maluynma T, Obinata K. Kawasaki disease followed by hemophagocytic syndrome. Eur J Pediatr. 1998; 157:610–611. PMID: 9686831.8. Ohga S, Ooshima A, Fukushige A, Ueda K. Histiocytic hemophagocytosis in a patient with Kawasaki disease: changes in the hypercytokinaemic state. Eur J Pediatr. 1995; 154:539–541. PMID: 7556319.9. Cummings C, McCarthy P, van Hoff J, Porter G. Kawasaki disease associated with reactive hemophagocytic lymphohistiocytosis. Pediatr Infect Dis J. 2008; 27:1116–1118. PMID: 18946363.
Article10. Titze U, Janka G, Schneider EM, Prall F, Haffner D, Classen CF. Hemophagocytic lymphohistiocytosis and Kawasaki disease: combined manifestation and differential diagnosis. Pediatr Blood Cancer. 2009; 53:493–495. PMID: 19434728.
Article11. Kim HK, Kim HG, Cho SJ, et al. Clinical characteristics of hemophagocytic lymphohistiocytosis related to Kawasaki disease. Pediatr Hematol Oncol. 2011; 28:230–236. PMID: 21381871.
Article12. Wang CL, Wu YT, Liu CA, Kuo HC, Yang KD. Kawasaki disease: infection, immunity and genetics. Pediatr Infect Dis J. 2005; 24:998–1004. PMID: 16282937.13. Asano T, Sudoh M, Watanabe M, Fujino O. Transient thrombocytopenia with large platelets in Kawasaki disease. Pediatr Hematol Oncol. 2007; 24:551–554. PMID: 17786792.
Article14. Filipovich AH. Hemophagocytic lymphohistiocytosis (HLH) and related disorders. Hematology Am Soc Hematol Educ Program. 2009; 127–131. PMID: 20008190.
Article15. Kim SY, Yoon JY, Lee SJ, et al. The clinical manifestations of hemophagocytic lymphohistiocytosis. Korean J Pediatr Hematol Oncol. 2003; 10:244–254.16. Park YW. Epidemiology of Kawasaki disease in Korea. Korean J Pediatr. 2008; 51:452–456.
Article17. Lee HJ, Cho AR, Kim HS, Sohn S. Clinical Characteristics of recurrent Kawasaki disease. Korean J Pediatr. 2004; 47:879–883.18. Mouy R, Stephan JL, Pillet P, Haddad E, Hubert P, Prieur AM. Efficacy of cyclosporine A in the treatment of macrophage activation syndrome in juvenile arthritis. J Pediatr. 1996; 129:750–754. PMID: 8917244.19. Kim KJ, Kim KH, Lee TJ, Chun JK, Lyu CJ, Kim DS. Clinical characteristics and prognostic factors for survival in hemophagocytic lymphohistiocytosis. Korean J Pediatr. 2008; 51:299–306.
Article20. Park HS, Kim DY, Lee JH, et al. Clinical features of adult patients with secondary hemophagocytic lymphohistiocytosis from causes other than lymphoma: an analysis of treatment outcome and prognostic fact. Ann Hematol. 2012; 91:897–904. PMID: 22147006.21. Im HJ, Song JS, Bae KU, et al. Outcome of hemophagocytic lymphohistiocytosis treated with HLH-94/2004 in Korea. In : The 32nd world congress of the international society of hematology; 2008. 64:p. abst 127.22. Yoon HS, Kim HJ, Yoo KH, et al. The UNC13D gene is the predominant causative gene with recurrent splicing mutations in Korean patients with familial hemophagocytic lymphohistiocytosis. Haematologica. 2010; 95:622–626. PMID: 20015888.