Anesth Pain Med.
2016 Jan;11(1):80-84. 10.17085/apm.2016.11.1.80.
Vertebroplasty of compression fracture with prevertebral hematoma during treatment of postherpetic neuralgia: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Yonsei University, Wonju College of Medicine, Wonju, Korea.
- 2Kimchan Pain Clinic, Suwon, Korea. painhankr@naver.com
- KMID: 2169080
- DOI: http://doi.org/10.17085/apm.2016.11.1.80
Abstract
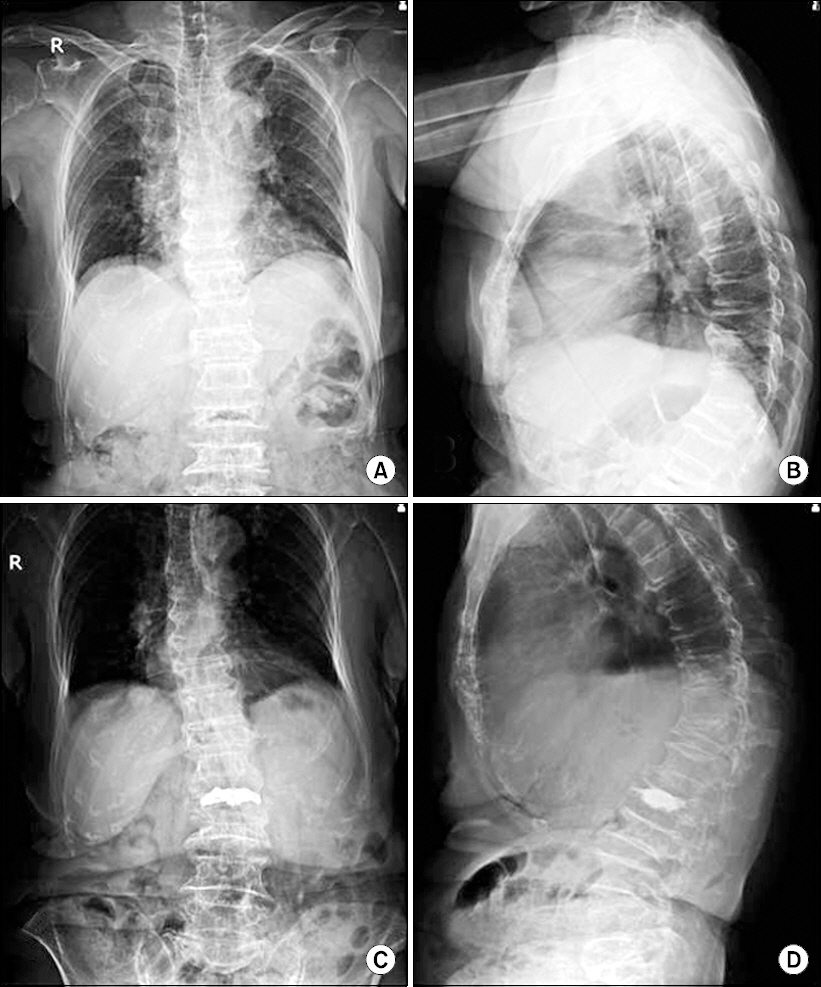
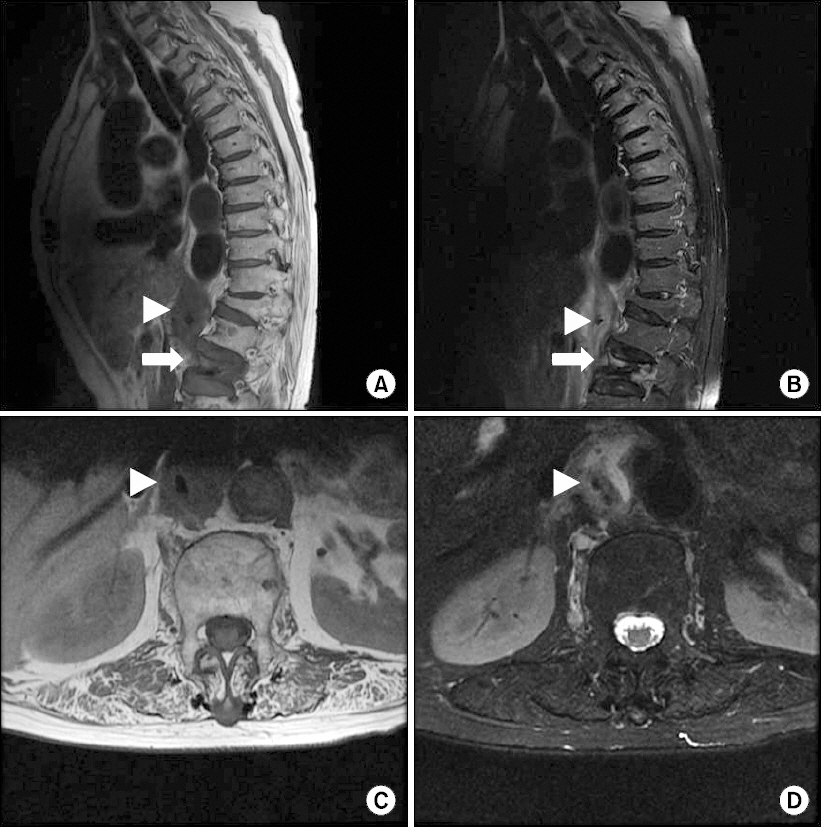
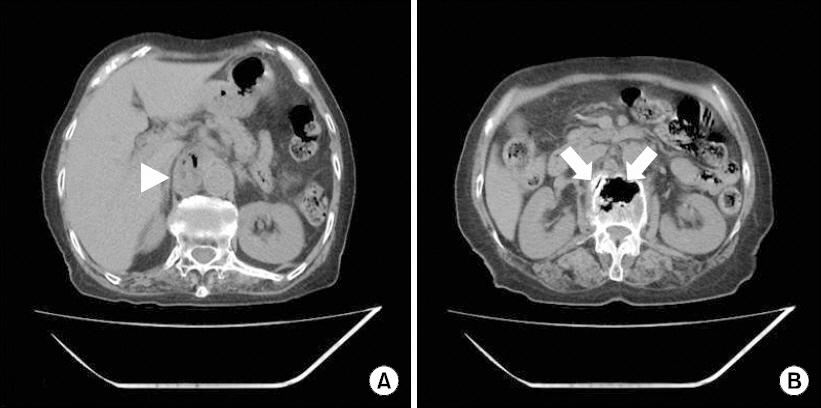
- Postherpetic neuralgia (PHN) and vertebral compression fracture (VCF) are common causes of chronic pain in the elderly population. Careful history taking and imaging studies are needed for diagnosis when both diseases coexist. Vertebroplasty is a clinically efficient surgical treatment of VCF, while nerve block and/or medications are the mainstay of PHN pain control. The most serious complications of vertebroplasty are pulmonary embolism or neurologic deficit due to cement leakage. An 80-year-old female patient was diagnosed with PHN of the right L1 dermatome; however, her pain expanded to the midback and subcostal area. Thoracic magnetic resonance imaging and abdominal computed tomography revealed recent L2 compression fracture with prevertebral hematoma caused by cortical bone defect of the L2 body. Even though the risk of cement leakage was high, L2 vertebral body augmentation was performed using a bone filler device and high-viscosity cement; this treatment was successful, without cement leakage or any other complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Nieuwenhuijse MJ, Van Erkel AR, Dijkstra PD. Cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: identification of risk factors. Spine J. 2011; 11:839–48. DOI: 10.1016/j.spinee.2011.07.027. PMID: 21889417.
Article2. Corcos G, Dbjay J, Mastier C, Leon S, Auperin A, De Baere T, et al. Cement leakage in percutaneous vertebroplasty for spinal metastases: a retrospective evaluation of incidence and risk factors. Spine (Phila Pa 1976). 2014; 39:332–8. DOI: 10.1097/BRS.0000000000000134. PMID: 24299719.3. Choi YM, Shin HY, Lee KJ, Koo MS, Nahm FS, Suh JH, et al. Compression fracture diagnosed during the treatment of postherpetic neuralgia. Korean J Pain. 2007; 20:224–9. DOI: 10.3344/kjp.2007.20.2.224.4. Hiwatashi A, Westesson PL, Yoshiura T, Noguchi T, Togao O, Yamashita K, et al. Kyphoplasty and vertebroplasty produce the same degree of height restoration. AJNR Am J Neuroradiol. 2009; 30:669–73. DOI: 10.3174/ajnr.A1442. PMID: 19131409.
Article5. Pradhan BB, Bae HW, Kropf MA, Patel VV, Delamarter RB. Kyphoplasty reduction of osteoporotic vertebral compression fractures: correction of local kyphosis versus overall sagittal alignment. Spine (Phila Pa 1976). 2006; 31:435–41. DOI: 10.1097/01.brs.0000200036.08679.1e. PMID: 16481954.
Article6. Weill A, Chiras J, Simon JM, Rose M, Sola-Martinez T, Enkaoua E. Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. Radiology. 1996; 199:241–7. DOI: 10.1148/radiology.199.1.8633152. PMID: 8633152.
Article7. Deramond H, Depriester C, Galibert P, Le Gars D. Percutaneous vertebroplasty with polymethylmethacrylate. Technique, indications, and results. Radiol Clin North Am. 1998; 36:533–46. DOI: 10.1016/S0033-8389(05)70042-7.8. Cosar M, Sasani M, Oktenoglu T, Kaner T, Ercelen O, Kose KC, et al. The major complications of transpedicular vertebroplasty. J Neurosurg Spine. 2009; 11:607–13. DOI: 10.3171/2009.4.SPINE08466. PMID: 19929366.
Article9. Heini PF, Orler R. Kyphoplasty for treatment of osteoporotic vertebral fractures. Eur Spine J. 2004; 13:184–92. DOI: 10.1007/s00586-003-0654-4. PMID: 14986073. PMCID: PMC3468137.10. Yang DH, Cho KH, Chung YS, Kim YR. Effect of vertebroplasty with bone filler device and compression with balloon kyphoplasty. Eur Spine J. 2014; 23:2718–25. DOI: 10.1007/s00586-014-3379-7. PMID: 24875381.11. Belkoff SM, Mathis JM, Jasper LE, Deramond H. The biomechanics of vertebroplasty. The effect of cement volume on mechanical behavior. Spine (Phila Pa 1976). 2001; 26:1537–41. DOI: 10.1097/00007632-200107150-00007.12. Hiwatashi A, Ohgiya Y, Kakimoto N, Westesson PL. Cement leakage during vertebroplasty can be predicted on preoperative MRI. AJR Am J Roentgenol. 2007; 188:1089–93. DOI: 10.2214/AJR.06.0903. PMID: 17377052.
Article13. Lee KH, Yoo DS, Kim YM, Lee YS. MR findings predictive of intradiscal leakage of bone cement in vertebroplasty. J Korean Radiol Soc. 2007; 56:371–7. DOI: 10.3348/jkrs.2007.56.4.371.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Onset of Spinal Subdural Hematoma after Vertebroplasty for Compression Fracture: A Case Report
- Compression Fractures Diagnosed during the Treatment of Postherpetic Neuralgia : A case report
- Root Injury after Percutaneous Vertebroplasty in Compression Fracture: Case Report
- Newly Developed Urinary Retention and Motor Weakness of Lower Extremities in a Postherpetic Neuralgia Patient
- Stuttering during Management of Postherpetic Neuralgia: A case report