Korean J Radiol.
2015 Oct;16(5):1079-1085. 10.3348/kjr.2015.16.5.1079.
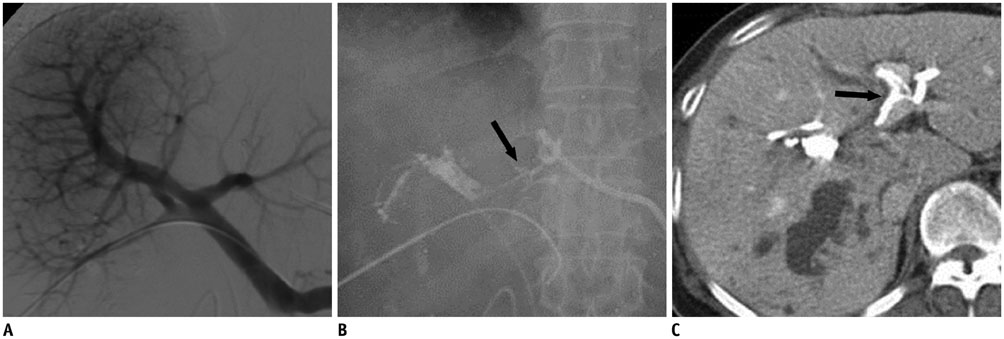
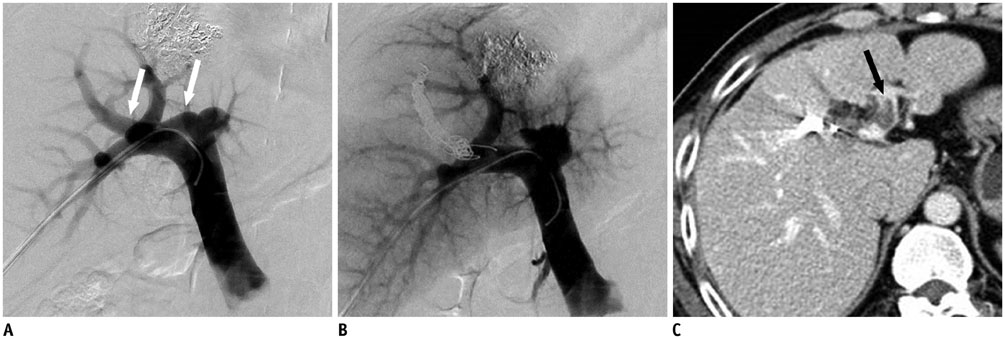
Complications of Portal Vein Embolization: Evaluation on Cross-Sectional Imaging
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 05505, Korea. jhshin@amc.seoul.kr
- KMID: 2160775
- DOI: http://doi.org/10.3348/kjr.2015.16.5.1079
Abstract
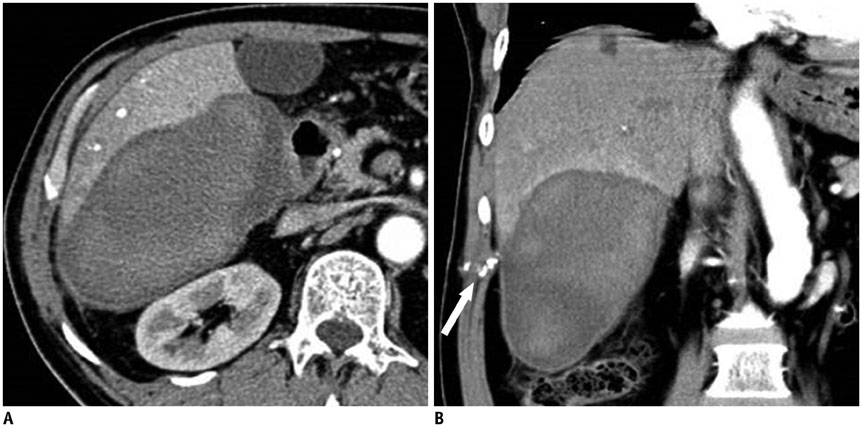
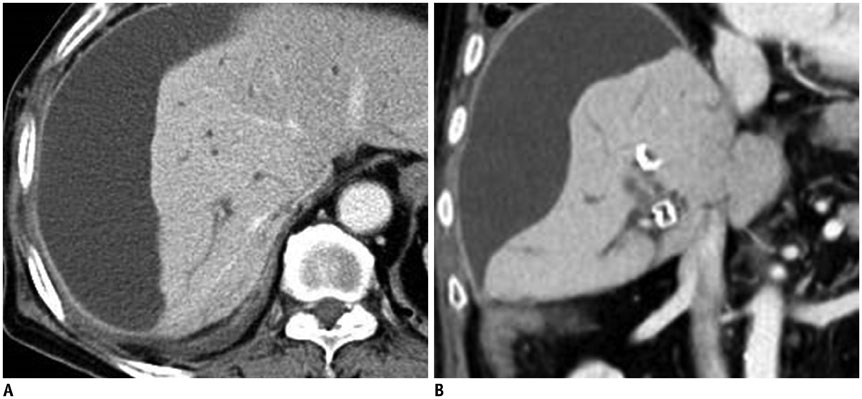
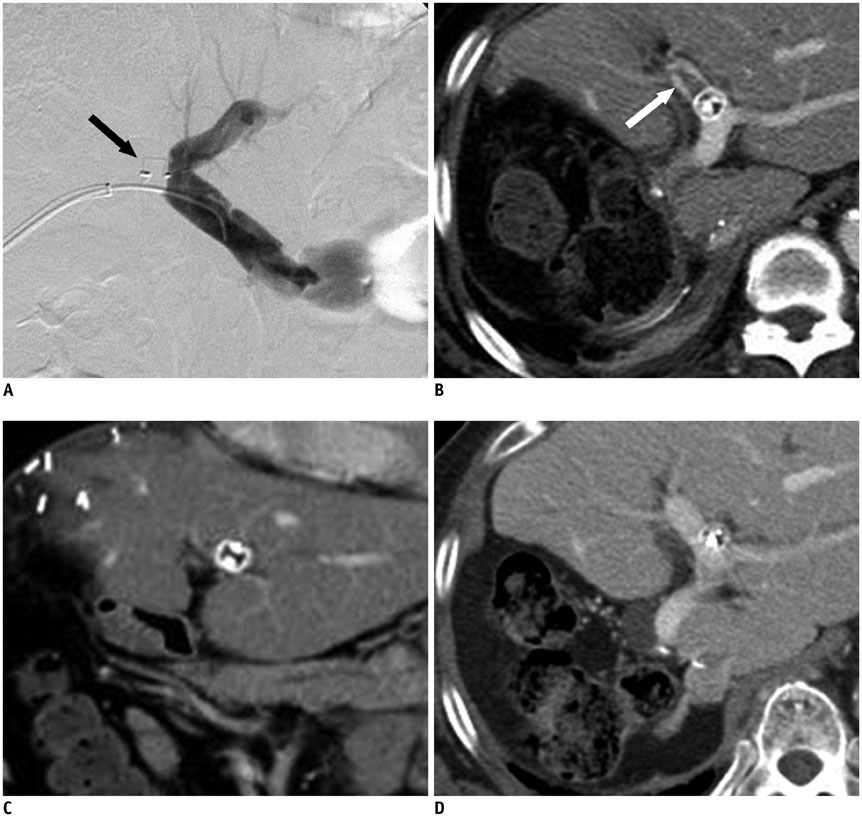
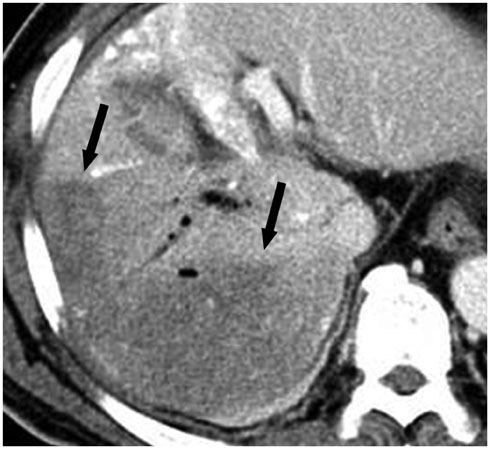
- Portal vein embolization (PVE) is known as an effective and safe preoperative procedure that increases the future liver remnant (FLR) in patients with insufficient FLR. However, some possible major complications can lead to non-resectability or delayed elective surgery that results in increased morbidity and mortality. Although the majority of these complications are rare, knowledge of the radiologic findings of post-procedural complications facilitate an accurate diagnosis and ensure prompt management. We accordingly reviewed the CT findings of the complications of PVE.
Keyword
MeSH Terms
Figure
Reference
-
1. Shindoh J, Tzeng CW, Aloia TA, Curley SA, Zimmitti G, Wei SH, et al. Portal vein embolization improves rate of resection of extensive colorectal liver metastases without worsening survival. Br J Surg. 2013; 100:1777–1783.2. May BJ, Talenfeld AD, Madoff DC. Update on portal vein embolization: evidence-based outcomes, controversies, and novel strategies. J Vasc Interv Radiol. 2013; 24:241–254.3. Azoulay D, Castaing D, Krissat J, Smail A, Hargreaves GM, Lemoine A, et al. Percutaneous portal vein embolization increases the feasibility and safety of major liver resection for hepatocellular carcinoma in injured liver. Ann Surg. 2000; 232:665–672.4. May BJ, Madoff DC. Portal vein embolization: rationale, technique, and current application. Semin Intervent Radiol. 2012; 29:81–89.5. Di Stefano DR, de Baere T, Denys A, Hakime A, Gorin G, Gillet M, et al. Preoperative percutaneous portal vein embolization: evaluation of adverse events in 188 patients. Radiology. 2005; 234:625–630.6. van Lienden KP, van den Esschert JW, de Graaf W, Bipat S, Lameris JS, van Gulik TM, et al. Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol. 2013; 36:25–34.7. Ganeshan DM, Szklaruk J. Portal vein embolization: cross-sectional imaging of normal features and complications. AJR Am J Roentgenol. 2012; 199:1275–1282.8. Park SY, Kim J, Kim BW, Wang HJ, Kim SS, Cheong JY, et al. Embolization of percutaneous transhepatic portal venous access tract with N-butyl cyanoacrylate. Br J Radiol. 2014; 87:20140347.9. Yokoyama Y, Ebata T, Igami T, Sugawara G, Mizuno T, Nagino M. The adverse effects of preoperative cholangitis on the outcome of portal vein embolization and subsequent major hepatectomies. Surgery. 2014; 156:1190–1196.10. Cho YK, Chang NK, Ma JS. Successful transcatheter closure of a large patent ductus venosus with the Amplatzer vascular plug II. Pediatr Cardiol. 2009; 30:540–542.11. Ratnam LA, Walkden RM, Munneke GJ, Morgan RA, Belli AM. The Amplatzer vascular plug for large vessel occlusion in the endovascular management of aneurysms. Eur Radiol. 2008; 18:2006–2012.12. Holbert BL, Baron RL, Dodd GD 3rd. Hepatic infarction caused by arterial insufficiency: spectrum and evolution of CT findings. AJR Am J Roentgenol. 1996; 166:815–820.13. Shaw CM, Madoff DC. Acute Thrombosis of Left Portal Vein during Right Portal Vein Embolization Extended to Segment 4. Semin Intervent Radiol. 2011; 28:156–161.14. Huang JY, Yang WZ, Li JJ, Jiang N, Zheng QB. Portal vein embolization induces compensatory hypertrophy of remnant liver. World J Gastroenterol. 2006; 12:408–414.15. Bilbao JI, Martínez-Cuesta A, Urtasun F, Cosín O. Complications of embolization. Semin Intervent Radiol. 2006; 23:126–142.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hemoperitoneum due to Ruptured Paraumbilical Vein in a Cirrhotic Patient with Portal Hypertension: Treatment by means of Coil Embolization
- Portal vein embolization in intrahepatic portal vein injury after blunt trauma: a case report
- Balloon Occlusion Retrograde Transvenous Obliteration of Gastric Varices in Two Non-Cirrhotic Patients with Portal Vein Thrombosis
- Blood flow volume difference (P-SS) between the portal vein and thesum of splenic vein and superior mesenteric vein in portal hypertension
- Congenital Portal Vein Aneurysm: A case report