J Korean Ophthalmol Soc.
2015 Dec;56(12):1985-1990. 10.3341/jkos.2015.56.12.1985.
A Case of Bilateral Diabetic Papillopathy Related to Rapid Hemoglobin A1c Decrease in Type I Diabetes Mellitus
- Affiliations
-
- 1Department of Ophthalmology, Myongji Hospital, Seonam University College of Medicine, Goyang, Korea. Kimdk89@empas.com
- KMID: 2148766
- DOI: http://doi.org/10.3341/jkos.2015.56.12.1985
Abstract
- PURPOSE
To report a case of bilateral diabetic papillopathy related to rapid hemoglobin A1c (HbA1c) decrease in a type I diabetic patient.
CASE SUMMARY
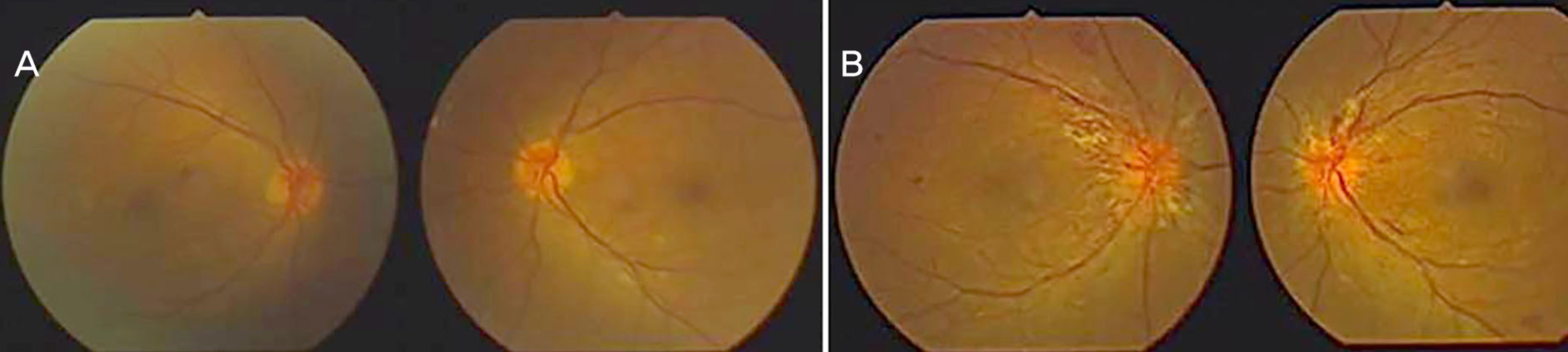
A 39-year-old female who was diagnosed with type I diabetes mellitus for the first time at this hospital was presented to our clinic for evaluation of diabetic retinopathy. There were no subjective symptoms, including blurred vision or visual defect. Her best corrected visual acuity in both eyes was 1.0, but her fundus resembled mild nonproliferative diabetic retinopathy. When diagnosed with type I diabetes mellitus, her HbA1c was 15.3%. She used insulin to control her blood glucose and her HbA1c reached 7.3% two months after controlling the blood glucose. Three months after her diabetic diagnosis, there were no differences in subjective symptoms and best corrected visual acuity. Fundus examination showed optic disc swelling in both eyes. To evaluate for the etiology of optic disc swelling, we did the examinations of the optic disc, fundus, and brain magnetic resonance imaging. No specific signs were observed. We diagnosed diabetic papillopathy and observed the patient without any treatments. Her optic disc swelling showed gradual improvement.
CONCLUSIONS
This case shows that the rapid HbA1c decrease in type I diabetes mellitus is related to the occurrence of bilateral diabetic papillopathy. This supports previous studies that estimated that the rapid HbA1c decrease in type I diabetes mellitus in response to insulin treatment is one of the risk factors for bilateral diabetic papillopathy.
MeSH Terms
Figure
Reference
-
References
1. Regillo CD, Brown GC, Savino PJ. . Diabetic papillopathy. Patient characteristics and fundus findings. Arch Ophthalmol. 1995; 113:889–95.
Article2. Ornek K, Oğ urel T. Intravitreal bevacizumab for diabetic papillopathy. J Ocul Pharmacol Ther. 2010; 26:217–8.3. Al-Haddad CE, Jurdi FA, Bashshur ZF. Intravitreal triamcinolone acetonide for the management of diabetic papillopathy. Am J Ophthalmol. 2004; 137:1151–3.
Article4. Appen RE, Chandra SR, Klein R, Myers FL. Diabetic papillopathy. Am J Ophthalmol. 1980; 90:203–9.
Article5. Mansour AM, El-Dairi MA, Shehab MA. . Periocular cortico-steroids in diabetic papillopathy. Eye (Lond). 2005; 19:45–51.
Article6. Shin JH, Choi KS. Intravitreal bevacizumab injection in diabetic papillopathy. J Korean Ophthalmol Soc. 2013; 54:1298–302.
Article7. Kim JJ, Im JC, Shin JP. . Two cases of long-term changes in the retinal nerve fiber layer thickness after intravitreal bevacizumab for diabetic papillopathy. J Korean Ophthalmol Soc. 2013; 54:1445–51.
Article8. Ostri C, Lund-Andersen H, Sander B. . Bilateral diabetic pap-illopathy and metabolic control. Ophthalmology. 2010; 117:2214–7.
Article9. Lubow M, Makley TA Jr. Pseudopapilledema of juvenile diabetes mellitus. Arch Ophthalmol. 1971; 85:417–22.
Article10. Cogan DG, Toussaint D, Kuwabara T. Retinal vascular patterns. IV. Diabetic retinopathy. Arch Ophthalmol. 1961; 66:366–78.11. Scott DJ, Dollery CT, Hill DW. . Fluorescein studies of the reti-nal circulation in diabetics. Br J Ophthalmol. 1963; 47:588–9.
Article12. Barr CC, Glaser JS, Blankenship G. Acute disc swelling in juvenile diabetes. Clinical profile and natural history of 12 cases. Arch Ophthalmol. 1980; 98:2185–92.13. Pavan PR, Aiello LM, Wafai MZ. . Optic disc edema in juve-nile-onset diabetes. Arch Ophthalmol. 1980; 98:2193–5.
Article14. Bayraktar Z, Alacali N, Bayraktar S. Diabetic papillopathy in type II diabetic patients. Retina. 2002; 22:752–8.
Article15. Hayreh SS, Zimmerman MB. Nonarteritic anterior ischemic optic neuropathy: clinical characteristics in diabetic patients versus non-diabetic patients. Ophthalmology. 2008; 115:1818–25.
Article16. Lauritzen T, Frost-Larsen K, Larsen HW, Deckert T. Effect of 1 year near-normal blood glucose levels on retinopathy in in-sulin-dependent diabetics. Lancet. 1983; 1:200–4.17. Early worsening of diabetic retinopathy in the Diabetes Control and Complications Trial Arch Ophthalmol. 1998; 116:874–86.18. Grunwald JE, Brucker AJ, Braunstein SN. . Strict metabolic control and retinal blood flow in diabetes mellitus. Br J Ophthalmol. 1994; 78:598–604.
Article19. Larsen M. Unilateral macular oedema secondary to retinal venous congestion without occlusion in patients with diabetes mellitus. Acta Ophthalmol Scand. 2005; 83:428–35.
Article20. Hayreh SS. Anterior ischemic optic neuropathy. Arch Neurol. 1981; 38:675–8.
Article21. Heller SR, Tattersall RB. Optic disc swelling in young diabetic pa-tients: a diagnostic dilemma. Diabet Med. 1987; 4:260–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Glycemic Control and Diabetic Retinopathy
- Acute Painful Neuropathy (Insulin Neuritis) in a Woman Following Rapid Glycemic Control for Type I Diabetes Mellitus
- The Optimal Cutoff Value of Glycated Hemoglobin for Detection of Diabetic Retinopathy
- The Study Related to Perceived Stress, Stress Coping Method, Self-Care Behavior and Hemoglobin A1c of Elderly Diabetic Mellitus Patients
- The Roles of Glycated Albumin as Intermediate Glycation Index and Pathogenic Protein