J Korean Neurosurg Soc.
2015 Jul;58(1):83-88. 10.3340/jkns.2015.58.1.83.
Growing Organized Hematomas Following Gamma Knife Radiosurgery for Cerebral Arteriovenous Malformation : Five Cases of Surgical Excision
- Affiliations
-
- 1Department of Neurosurgery, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea. jsahn@amc.seoul.kr
- KMID: 2067111
- DOI: http://doi.org/10.3340/jkns.2015.58.1.83
Abstract
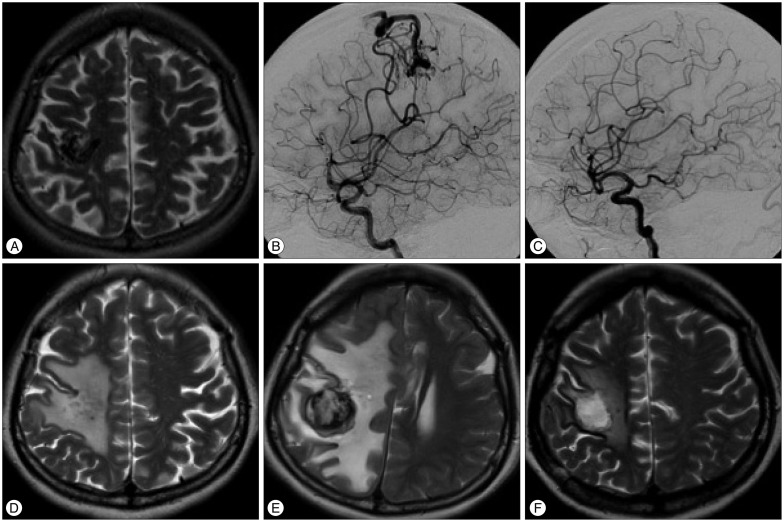
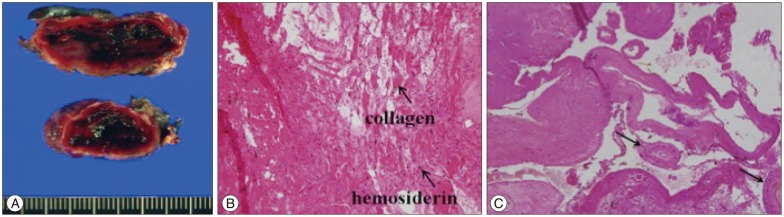
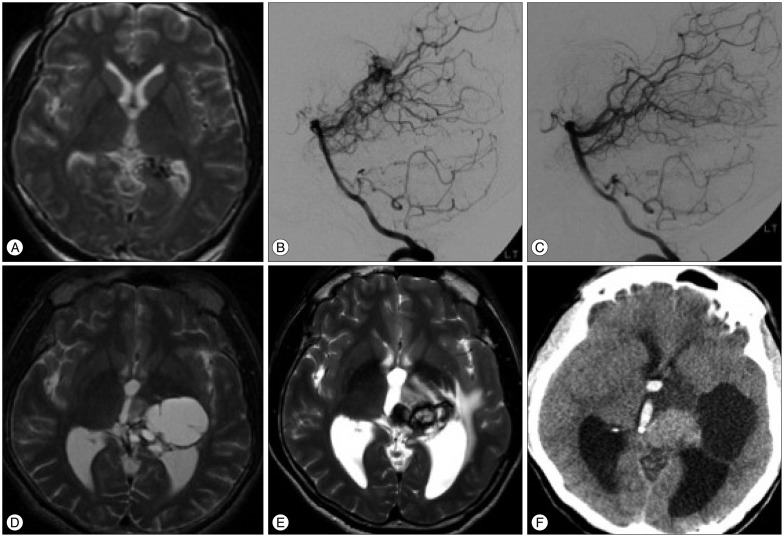
- Organized hematoma is a rare complication that can develop following gamma knife radiosurgery (GKS) for cerebral arteriovenous malformation (AVM). Here, we describe 5 patients with growing organized hematomas that developed from completely obliterated AVMs several years after GKS. The patients were 15, 16, 30, 36, and 38 years old at the time of GKS, respectively, and 3 patients were female. Four AVMs were located in the lobe of the brain, and the remaining AVM were in the thalamus. Between 2-12 years after GKS, patients developed progressive symptoms such intractable headache or hemiparesis and enhancing mass lesions were identified. Follow-up visits revealed the slow expansion of the hematomas and surrounding edema. Steroids were ineffective, and thus surgery was performed. Histology revealed organized hematomas with a capsule, but there was no evidence of residual AVMs or vascular malformation. After surgery, the neurological symptoms of all patients improved and the surrounding edema resolved. However, the hematoma continued to expand and intraventricular hemorrhage developed in 1 patient whose hematoma was only partially removed. GKS for cerebral AVM can be complicated by growing, organized hematomas that develop after complete obliteration. Growing hematomas should be surgically evacuated if they are symptomatic. Radical resection of the hematoma capsule is also strongly recommended.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Radiosurgery for Cerebral Arteriovenous Malformation (AVM) : Current Treatment Strategy and Radiosurgical Technique for Large Cerebral AVM
Joonho Byun, Do Hoon Kwon, Do Heui Lee, Wonhyoung Park, Jung Cheol Park, Jae Sung Ahn
J Korean Neurosurg Soc. 2020;63(4):415-426. doi: 10.3340/jkns.2020.0008.
Reference
-
1. Al Hinai Q, Tampieri D, Souhami L, Sadikot A, Sinclair D, Leblanc R. Cyst formation following radiosurgery for AVMs : report of 3 cases. Can J Neurol Sci. 2011; 38:734–740. PMID: 21856577.2. Clark AJ, Butowski NA, Chang SM, Prados MD, Clarke J, Polley MY, et al. Impact of bevacizumab chemotherapy on craniotomy wound healing. J Neurosurg. 2011; 114:1609–1616. PMID: 21142749.
Article3. Hirsh LF, Spector HB, Bogdanoff BM. Chronic encapsulated intracerebral hematoma. Neurosurgery. 1981; 9:169–172. PMID: 7266817.
Article4. Izawa M, Chernov M, Hayashi M, Nakaya K, Kamikawa S, Kato K, et al. Management and prognosis of cysts developed on long-term follow-up after Gamma Knife radiosurgery for intracranial arteriovenous malformations. Surg Neurol. 2007; 68:400–406. discussion 406PMID: 17905064.
Article5. Kaido T, Hoshida T, Uranishi R, Akita N, Kotani A, Nishi N, et al. Radiosurgery-induced brain tumor. Case report. J Neurosurg. 2001; 95:710–713. PMID: 11596968.6. Kurita H, Sasaki T, Kawamoto S, Taniguchi M, Kitanaka C, Nakaguchi H, et al. Chronic encapsulated expanding hematoma in association with gamma knife stereotactic radiosurgery for a cerebral arteriovenous malformation. Case report. J Neurosurg. 1996; 84:874–878. PMID: 8622164.
Article7. Lee CC, Pan DH, Ho DM, Wu HM, Chung WY, Liu KD, et al. Chronic encapsulated expanding hematoma after gamma knife stereotactic radiosurgery for cerebral arteriovenous malformation. Clin Neurol Neurosurg. 2011; 113:668–671. PMID: 21507569.
Article8. Maruyama K, Shin M, Tago M, Kurita H, Kawahara N, Morita A, et al. Management and outcome of hemorrhage after Gamma Knife surgery for arteriovenous malformations of the brain. J Neurosurg. 2006; 105(Suppl):52–57. PMID: 18503330.
Article9. Motegi H, Kuroda S, Ishii N, Aoyama H, Terae S, Shirato H, et al. De novo formation of cavernoma after radiosurgery for adult cerebral arteriovenous malformation--case report. Neurol Med Chir (Tokyo). 2008; 48:397–400. PMID: 18812682.
Article10. Nakamizo A, Suzuki SO, Saito N, Shono T, Matsumoto K, Onaka S, et al. Clinicopathological study on chronic encapsulated expanding hematoma associated with incompletely obliterated AVM after stereotactic radiosurgery. Acta Neurochir (Wien). 2011; 153:883–893. PMID: 20931239.
Article11. Pozzati E, Giuliani G, Gaist G, Piazza G, Vergoni G. Chronic expanding intracerebral hematoma. J Neurosurg. 1986; 65:611–614. PMID: 3772447.
Article12. Roda JM, Carceller F, Pérez-Higueras A, Morales C. Encapsulated intracerebral hematomas : a defined entity. Case report. J Neurosurg. 1993; 78:829–833. PMID: 8468616.13. Shuto T, Matsunaga S, Suenaga J. Surgical treatment for late complications following gamma knife surgery for arteriovenous malformations. Stereotact Funct Neurosurg. 2011; 89:96–102. PMID: 21293169.
Article14. Shuto T, Ohtake M, Matsunaga S. Proposed mechanism for cyst formation and enlargement following Gamma Knife Surgery for arteriovenous malformations. J Neurosurg. 2012; 117(Suppl):135–143. PMID: 23205801.
Article15. Takeuchi S, Takasato Y, Masaoka H. Chronic encapsulated intracerebral hematoma formation after radiosurgery for cerebral arteriovenous malformation. Neurol India. 2011; 59:624–626. PMID: 21891948.
Article16. Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yoshino Y, et al. Development of chronic encapsulated intracerebral hematoma after radiosurgery for a cerebral arteriovenous malformation. Acta Neurochir (Wien). 2009; 151:1513–1515. PMID: 19597762.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recurrence of pediatric cerebral arteriovenous malformation after obliteration by radiosurgery: a case report
- Cyst Formation after Gamma Knife Radiosurgery for Cerebral Arteriovenous Malformation
- Delayed Perilesional Ischemic Stroke after Gamma-knife Radiosurgery for Unruptured Deep Arteriovenous Malformation: Two Case Reports of Radiation-induced Small Artery Injury as Possible Cause
- Gamma Knife Radiosurgery in Cerebral Arteriovenous Malformation
- Huge Cyst Formation after Gamma Knife Radiosurgery for Arteriovenous Malformation: A Case Report