Korean J Urol.
2011 Oct;52(10):715-717. 10.4111/kju.2011.52.10.715.
Unusual Presentation of Bilateral Adrenocortical Carcinoma Mimicking Adrenal Metastasis
- Affiliations
-
- 1Department of Urology, Chonbuk National University Medical School, Jeonju, Korea. mkkim@chonbuk.ac.kr
- 2Department of Urology, Chosun University College of Medicine, Gwangju, Korea.
- KMID: 2061436
- DOI: http://doi.org/10.4111/kju.2011.52.10.715
Abstract
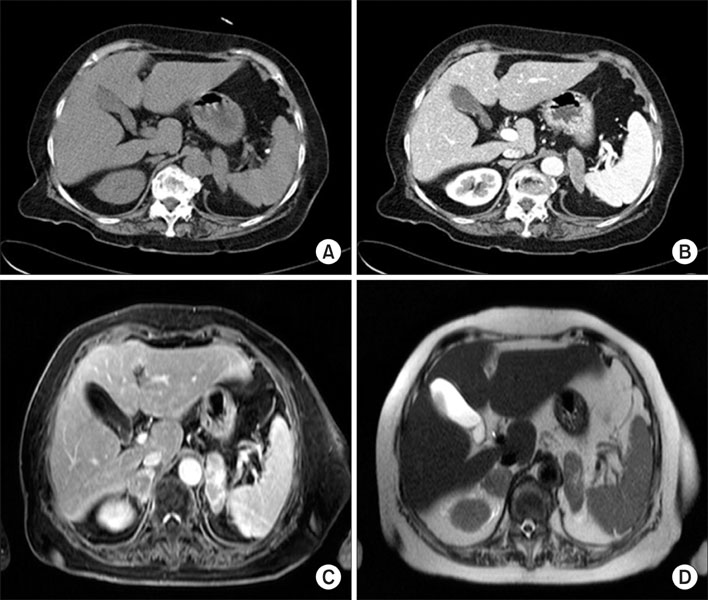
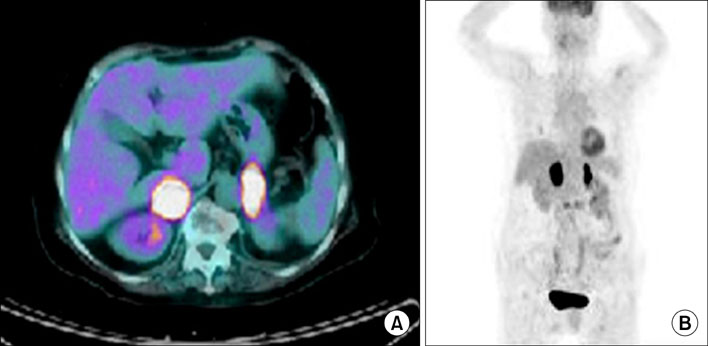
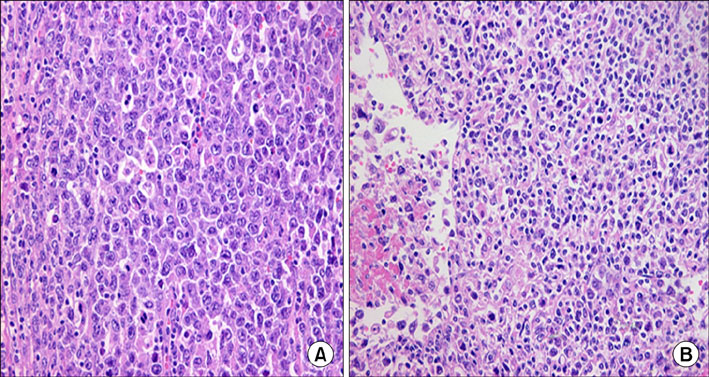
- A 75-year-old female visited our hospital with bilateral adrenal masses that were detected incidentally during lumbar spine magnetic resonance imaging (MRI) for the evaluation of radiating flank pain. Consecutive computed tomography and MRI revealed bilateral adrenal masses with no evidence of lymph node enlargement or local invasion; 2[(18)F]fluoro-2-deoxyglucose (FDG)-positron emission tomography showed an intense FDG accumulation in both adrenal glands without abnormal FDG uptake in extra-adrenal regions. The laboratory test results were within normal ranges. We performed a bilateral adrenalectomy. The pathologic diagnosis of both adrenal masses was consistent with adrenocortical carcinoma. The patient recovered well with no complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Ozimek A, Diebold J, Linke R, Heyn J, Hallfeldt K, Mussack T. Bilateral primary adrenal non-Hodgkin's lymphoma and primary adrenocortical carcinoma-review of the literature preoperative differentiation of adrenal tumors. Endocr J. 2008. 55:625–638.2. Dunnick NR, Korobkin M. Imaging of adrenal incidentalomas: current status. AJR Am J Roentgenol. 2002. 179:559–568.3. Allolio B, Fassnacht M. Clinical review: Adrenocortical carcinoma: clinical update. J Clin Endocrinol Metab. 2006. 91:2027–2037.4. Mansmann G, Lau J, Balk E, Rothberg M, Miyachi Y, Bornstein SR. The clinically inapparent adrenal mass: update in diagnosis and management. Endocr Rev. 2004. 25:309–340.5. Pacak K, Eisenhofer G, Goldstein DS. Functional imaging of endocrine tumors: role of positron emission tomography. Endocr Rev. 2004. 25:568–580.6. Palazzo FF, Sebag F, Sierra M, Ippolito G, Souteyrand P, Henry JF. Long-term outcome following laparoscopic adrenalectomy for large solid adrenal cortex tumors. World J Surg. 2006. 30:893–898.7. Valeri A, Bergamini C, Manca G, Mannelli M, Presenti L, Peri A, et al. Adrenal incidentaloma: The influence of a decision-making algorithm on the short-term outcome of laparoscopy. J Laparoendosc Adv Surg Tech A. 2005. 15:451–459.8. Aiba M, Fujibayashi M. Histopathological diagnosis and prognostic factors in adrenocortical carcinoma. Endocr Pathol. 2005. 16:13–22.9. Weiss LM. Comparative histologic study of 43 metastasizing and nonmetastasizing adrenocortical tumors. Am J Surg Pathol. 1984. 8:163–169.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral nonfunctioning adrenocortical carcinoma: a case report
- A Case Report of Bilateral Adrenocortical Carcinoma Complicated by Adrenal Insufficiency
- A case of asynchromous bilateral nonfunctioning adrenal cortical carcinoma
- Spontaneous Rupture of Nonfunctioning Adrenocortical Carcinoma
- Imaging of F-18 FDG PET/CT and follow up of bilateral invasive adrenal diffuse large B cell lymphoma mimicking adrenocortical carcinoma