J Cardiovasc Ultrasound.
2014 Sep;22(3):101-110. 10.4250/jcu.2014.22.3.101.
A Primer on the Methods and Applications for Contrast Echocardiography in Clinical Imaging
- Affiliations
-
- 1Knight Cardiovascular Institute, Oregon Health & Science University, Portland, OR, USA. lindnerj@ohsu.edu
- KMID: 2045424
- DOI: http://doi.org/10.4250/jcu.2014.22.3.101
Abstract
- Contrast echocardiography is broadly described as a variety of techniques whereby the blood pool on cardiac ultrasound is enhanced with encapsulated gas-filled microbubbles or other acoustically active nano- or microparticles. The development of this technology has occurred primarily in response to the need improve current diagnostic applications of echocardiography such as the need to better define left ventricular cavity volumes, regional wall motion, or the presence or absence of masses and thrombi. A secondary reason for the development of contrast echocardiography has been to expand the capabilities of echocardiography. These new applications include myocardial perfusion imaging for detection of ischemia and viability, perfusion imaging of masses/tumors, and molecular imaging. The ability to fill all of these current and future clinical roles has been predicated on the ability to produce robust contrast signal which, in turn, has relied on technical innovation with regards to the microbubble contrast agents and the ultrasound imaging paradigms. In this review, we will discuss the basics of contrast echocardiography including the composition of microbubble contrast agents, the unique imaging methods used to optimize contrast signal-to-noise ratio, and the clinical applications of contrast echocardiography that have made a clinical impact.
MeSH Terms
Figure
Reference
-
1. Kaufmann BA, Wei K, Lindner JR. Contrast echocardiography. Curr Probl Cardiol. 2007; 32:51–96.
Article2. Hoffmann R, von Bardeleben S, ten Cate F, Borges AC, Kasprzak J, Firschke C, Lafitte S, Al-Saadi N, Kuntz-Hehner S, Engelhardt M, Becher H, Vanoverschelde JL. Assessment of systolic left ventricular function: a multi-centre comparison of cineventriculography, cardiac magnetic resonance imaging, unenhanced and contrast-enhanced echocardiography. Eur Heart J. 2005; 26:607–616.
Article3. Thomson HL, Basmadjian AJ, Rainbird AJ, Razavi M, Avierinos JF, Pellikka PA, Bailey KR, Breen JF, Enriquez-Sarano M. Contrast echocardiography improves the accuracy and reproducibility of left ventricular remodeling measurements: a prospective, randomly assigned, blinded study. J Am Coll Cardiol. 2001; 38:867–875.
Article4. Reilly JP, Tunick PA, Timmermans RJ, Stein B, Rosenzweig BP, Kronzon I. Contrast echocardiography clarifies uninterpretable wall motion in intensive care unit patients. J Am Coll Cardiol. 2000; 35:485–490.
Article5. Kurt M, Shaikh KA, Peterson L, Kurrelmeyer KM, Shah G, Nagueh SF, Fromm R, Quinones MA, Zoghbi WA. Impact of contrast echocardiography on evaluation of ventricular function and clinical management in a large prospective cohort. J Am Coll Cardiol. 2009; 53:802–810.
Article6. Thavendiranathan P, Grant AD, Negishi T, Plana JC, Popović ZB, Marwick TH. Reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection fraction and volumes: application to patients undergoing cancer chemotherapy. J Am Coll Cardiol. 2013; 61:77–84.
Article7. Plana JC, Mikati IA, Dokainish H, Lakkis N, Abukhalil J, Davis R, Hetzell BC, Zoghbi WA. A randomized cross-over study for evaluation of the effect of image optimization with contrast on the diagnostic accuracy of dobutamine echocardiography in coronary artery disease The OPTIMIZE Trial. JACC Cardiovasc Imaging. 2008; 1:145–152.
Article8. Thanigaraj S, Nease RF Jr, Schechtman KB, Wade RL, Loslo S, Pérez JE. Use of contrast for image enhancement during stress echocardiography is cost-effective and reduces additional diagnostic testing. Am J Cardiol. 2001; 87:1430–1432.
Article9. Crouse LJ, Cheirif J, Hanly DE, Kisslo JA, Labovitz AJ, Raichlen JS, Schutz RW, Shah PM, Smith MD. Opacification and border delineation improvement in patients with suboptimal endocardial border definition in routine echocardiography: results of the Phase III Albunex Multicenter Trial. J Am Coll Cardiol. 1993; 22:1494–1500.
Article10. Rainbird AJ, Mulvagh SL, Oh JK, McCully RB, Klarich KW, Shub C, Mahoney DW, Pellikka PA. Contrast dobutamine stress echocardiography: clinical practice assessment in 300 consecutive patients. J Am Soc Echocardiogr. 2001; 14:378–385.
Article11. Siebelink HM, Scholte AJ, Van de Veire NR, Holman ER, Nucifora G, van der Wall EE, Bax JJ. Value of contrast echocardiography for left ventricular thrombus detection postinfarction and impact on antithrombotic therapy. Coron Artery Dis. 2009; 20:462–466.
Article12. Bezante GP, Chen X, Molinari G, Valbusa A, Deferrari L, Sebastiani V, Yokoyama N, Steinmetz S, Barsotti A, Schwarz KQ. Left ventricular myocardial mass determination by contrast enhanced colour Doppler compared with magnetic resonance imaging. Heart. 2005; 91:38–43.
Article13. Soman P, Swinburn J, Callister M, Stephens NG, Senior R. Apical hypertrophic cardiomyopathy: bedside diagnosis by intravenous contrast echocardiography. J Am Soc Echocardiogr. 2001; 14:311–313.
Article14. Moon JC, Fisher NG, McKenna WJ, Pennell DJ. Detection of apical hypertrophic cardiomyopathy by cardiovascular magnetic resonance in patients with non-diagnostic echocardiography. Heart. 2004; 90:645–649.
Article15. Koo BK, Choi D, Ha JW, Kang SM, Chung N, Cho SY. Isolated noncompaction of the ventricular myocardium: contrast echocardiographic findings and review of the literature. Echocardiography. 2002; 19:153–156.
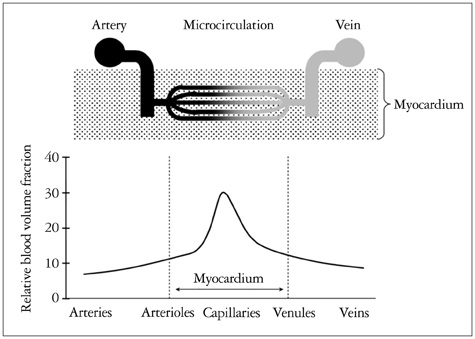
Article16. Kassab GS, Lin DH, Fung YC. Morphometry of pig coronary venous system. Am J Physiol. 1994; 267(6 Pt 2):H2100–H2113.
Article17. Lindner JR, Villanueva FS, Dent JM, Wei K, Sklenar J, Kaul S. Assessment of resting perfusion with myocardial contrast echocardiography: theoretical and practical considerations. Am Heart J. 2000; 139(2 Pt 1):231–240.
Article18. Balcells E, Powers ER, Lepper W, Belcik T, Wei K, Ragosta M, Samady H, Lindner JR. Detection of myocardial viability by contrast echocardiography in acute infarction predicts recovery of resting function and contractile reserve. J Am Coll Cardiol. 2003; 41:827–833.
Article19. Main ML, Magalski A, Chee NK, Coen MM, Skolnick DG, Good TH. Full-motion pulse inversion power Doppler contrast echocardiography differentiates stunning from necrosis and predicts recovery of left ventricular function after acute myocardial infarction. J Am Coll Cardiol. 2001; 38:1390–1394.
Article20. Shimoni S, Frangogiannis NG, Aggeli CJ, Shan K, Quinones MA, Espada R, Letsou GV, Lawrie GM, Winters WL, Reardon MJ, Zoghbi WA. Microvascular structural correlates of myocardial contrast echocardiography in patients with coronary artery disease and left ventricular dysfunction: implications for the assessment of myocardial hibernation. Circulation. 2002; 106:950–956.
Article21. Janardhanan R, Moon JC, Pennell DJ, Senior R. Myocardial contrast echocardiography accurately reflects transmurality of myocardial necrosis and predicts contractile reserve after acute myocardial infarction. Am Heart J. 2005; 149:355–362.
Article22. Rinkevich D, Kaul S, Wang XQ, Tong KL, Belcik T, Kalvaitis S, Lepper W, Dent JM, Wei K. Regional left ventricular perfusion and function in patients presenting to the emergency department with chest pain and no ST-segment elevation. Eur Heart J. 2005; 26:1606–1611.
Article23. Tong KL, Kaul S, Wang XQ, Rinkevich D, Kalvaitis S, Belcik T, Lepper W, Foster WA, Wei K. Myocardial contrast echocardiography versus Thrombolysis In Myocardial Infarction score in patients presenting to the emergency department with chest pain and a nondiagnostic electrocardiogram. J Am Coll Cardiol. 2005; 46:920–927.
Article24. Kaul S, Pandian NG, Guerrero JL, Gillam LD, Okada RD, Weyman AE. Effects of selectively altering collateral driving pressure on regional perfusion and function in occluded coronary bed in the dog. Circ Res. 1987; 61:77–85.
Article25. Piek JJ, Becker AE. Collateral blood supply to the myocardium at risk in human myocardial infarction: a quantitative postmortem assessment. J Am Coll Cardiol. 1988; 11:1290–1296.
Article26. Levin DC. Pathways and functional significance of the coronary collateral circulation. Circulation. 1974; 50:831–837.
Article27. Verma S, Fedak PW, Weisel RD, Butany J, Rao V, Maitland A, Li RK, Dhillon B, Yau TM. Fundamentals of reperfusion injury for the clinical cardiologist. Circulation. 2002; 105:2332–2336.
Article28. Elhendy A, O'Leary EL, Xie F, McGrain AC, Anderson JR, Porter TR. Comparative accuracy of real-time myocardial contrast perfusion imaging and wall motion analysis during dobutamine stress echocardiography for the diagnosis of coronary artery disease. J Am Coll Cardiol. 2004; 44:2185–2191.
Article29. Jeetley P, Hickman M, Kamp O, Lang RM, Thomas JD, Vannan MA, Vanoverschelde JL, van der Wouw PA, Senior R. Myocardial contrast echocardiography for the detection of coronary artery stenosis: a prospective multicenter study in comparison with single-photon emission computed tomography. J Am Coll Cardiol. 2006; 47:141–145.
Article30. Shimoni S, Zoghbi WA, Xie F, Kricsfeld D, Iskander S, Gobar L, Mikati IA, Abukhalil J, Verani MS, O'Leary EL, Porter TR. Real-time assessment of myocardial perfusion and wall motion during bicycle and treadmill exercise echocardiography: comparison with single photon emission computed tomography. J Am Coll Cardiol. 2001; 37:741–747.
Article31. Peltier M, Vancraeynest D, Pasquet A, Ay T, Roelants V, D'hondt AM, Melin JA, Vanoverschelde JL. Assessment of the physiologic significance of coronary disease with dipyridamole real-time myocardial contrast echocardiography. Comparison with technetium-99m sestamibi single-photon emission computed tomography and quantitative coronary angiography. J Am Coll Cardiol. 2004; 43:257–264.
Article32. Wei K, Crouse L, Weiss J, Villanueva F, Schiller NB, Naqvi TZ, Siegel R, Monaghan M, Goldman J, Aggarwal P, Feigenbaum H, DeMaria A. Comparison of usefulness of dipyridamole stress myocardial contrast echocardiography to technetium-99m sestamibi single-photon emission computed tomography for detection of coronary artery disease (PB127 Multicenter Phase 2 Trial results). Am J Cardiol. 2003; 91:1293–1298.
Article33. Leong-Poi H, Coggins MP, Sklenar J, Jayaweera AR, Wang XQ, Kaul S. Role of collateral blood flow in the apparent disparity between the extent of abnormal wall thickening and perfusion defect size during acute myocardial infarction and demand ischemia. J Am Coll Cardiol. 2005; 45:565–572.
Article34. Dodla S, Xie F, Smith M, O'Leary E, Porter TR. Real-time perfusion echocardiography during treadmill exercise and dobutamine stress testing. Heart. 2010; 96:220–225.
Article35. Sboros V, Moran CM, Anderson T, McDicken WN. An in vitro comparison of ultrasonic contrast agents in solutions with varying air levels. Ultrasound Med Biol. 2000; 26:807–818.
Article36. de Jong N, Hoff L, Skotland T, Bom N. Absorption and scatter of encapsulated gas filled microspheres: theoretical considerations and some measurements. Ultrasonics. 1992; 30:95–103.
Article37. Abdelmoneim SS, Mankad SV, Bernier M, Dhoble A, Hagen ME, Ness SA, Chandrasekaran K, Pellikka PA, Oh JK, Mulvagh SL. Microvascular function in Takotsubo cardiomyopathy with contrast echocardiography: prospective evaluation and review of literature. J Am Soc Echocardiogr. 2009; 22:1249–1255.
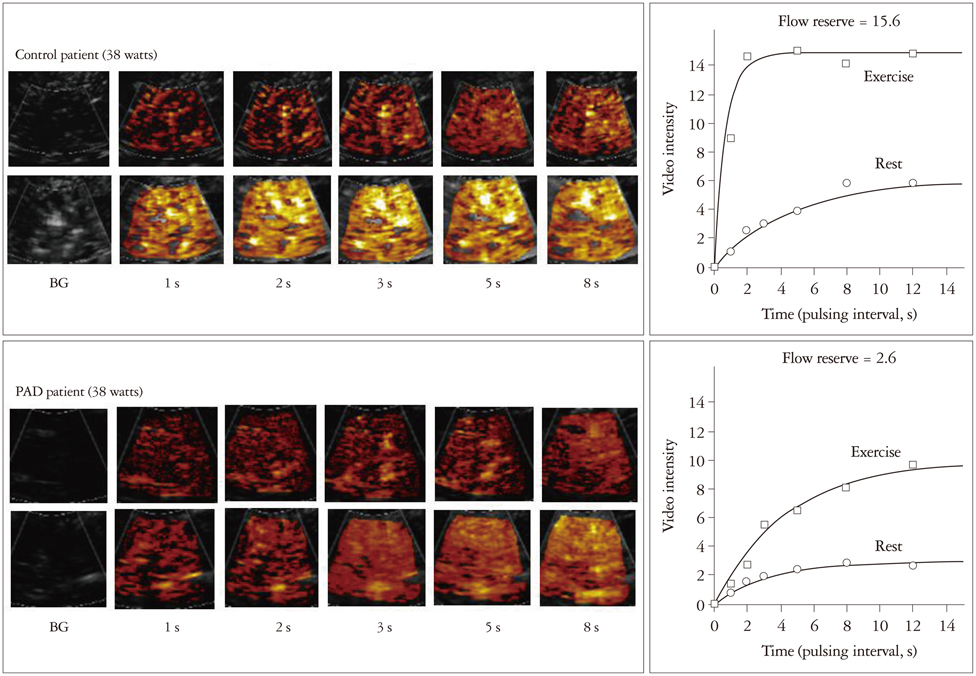
Article38. Lindner JR, Womack L, Barrett EJ, Weltman J, Price W, Harthun NL, Kaul S, Patrie JT. Limb stress-rest perfusion imaging with contrast ultrasound for the assessment of peripheral arterial disease severity. JACC Cardiovasc Imaging. 2008; 1:343–350.
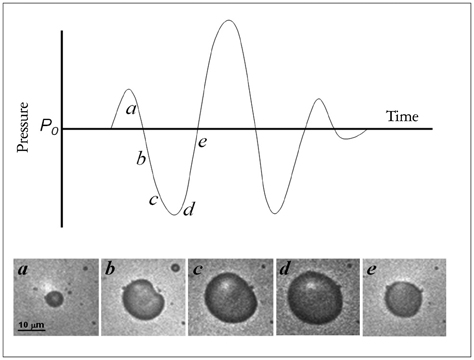
Article39. de Jong N, Frinking PJ, Bouakaz A, Goorden M, Schourmans T, Jingping X, Mastik F. Optical imaging of contrast agent microbubbles in an ultrasound field with a 100-MHz camera. Ultrasound Med Biol. 2000; 26:487–492.
Article40. Weissman NJ, Cohen MC, Hack TC, Gillam LD, Cohen JL, Kitzman DW. Infusion versus bolus contrast echocardiography: a multicenter, open-label, crossover trial. Am Heart J. 2000; 139:399–404.
Article41. Wei K, Jayaweera AR, Firoozan S, Linka A, Skyba DM, Kaul S. Basis for detection of stenosis using venous administration of microbubbles during myocardial contrast echocardiography: bolus or continuous infusion. J Am Coll Cardiol. 1998; 32:252–260.
Article42. Burns PN. Harmonic imaging with ultrasound contrast agents. Clin Radiol. 1996; 51:Suppl 1. 50–55.43. Porter TR, Xie F, Kricsfeld D, Armbruster RW. Improved myocardial contrast with second harmonic transient ultrasound response imaging in humans using intravenous perfluorocarbon-exposed sonicated dextrose albumin. J Am Coll Cardiol. 1996; 27:1497–1501.
Article44. Senior R, Kaul S, Soman P, Lahiri A. Power doppler harmonic imaging: a feasibility study of a new technique for the assessment of myocardial perfusion. Am Heart J. 2000; 139(2 Pt 1):245–251.
Article45. Kuersten B, Murthy TH, Li P, Liu Z, Locricchio E, Baisch C, Rafter P, Vannan M. Ultraharmonic myocardial contrast imaging: in vivo experimental and clinical data from a novel technique. J Am Soc Echocardiogr. 2001; 14:910–916.
Article46. Simpson DH, Chin CT, Burns PN. Pulse inversion Doppler: a new method for detecting nonlinear echoes from microbubble contrast agents. IEEE Trans Ultrason Ferroelectr Freq Control. 1999; 46:372–382.
Article47. Mor-Avi V, Caiani EG, Collins KA, Korcarz CE, Bednarz JE, Lang RM. Combined assessment of myocardial perfusion and regional left ventricular function by analysis of contrast-enhanced power modulation images. Circulation. 2001; 104:352–357.
Article48. Lindner JR, Song J, Jayaweera AR, Sklenar J, Kaul S. Microvascular rheology of Definity microbubbles after intra-arterial and intravenous administration. J Am Soc Echocardiogr. 2002; 15:396–403.
Article