J Breast Cancer.
2013 Dec;16(4):410-416. 10.4048/jbc.2013.16.4.410.
Survival Outcomes of Different Treatment Methods for the Ipsilateral Breast of Occult Breast Cancer Patients with Axillary Lymph Node Metastasis: A Single Center Experience
- Affiliations
-
- 1Division of Breast and Endocrine Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. brdrson@korea.com
- 2Department of Clinical Epidemiology and Biostatistics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 1976379
- DOI: http://doi.org/10.4048/jbc.2013.16.4.410
Abstract
- PURPOSE
This study compared the survival outcomes of different treatment methods for the ipsilateral breast of occult breast cancer (OBC) patients with axillary lymph node metastasis.
METHODS
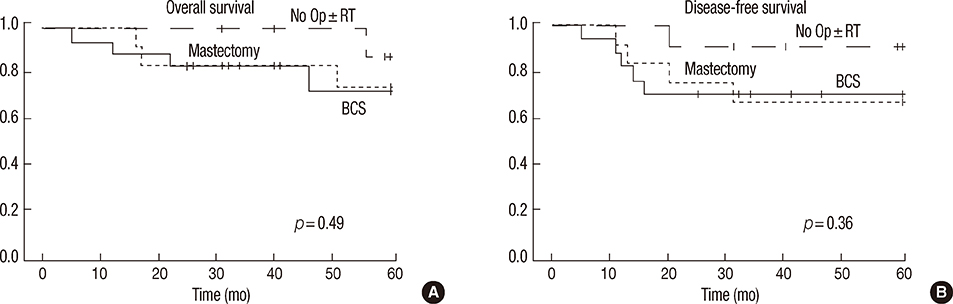
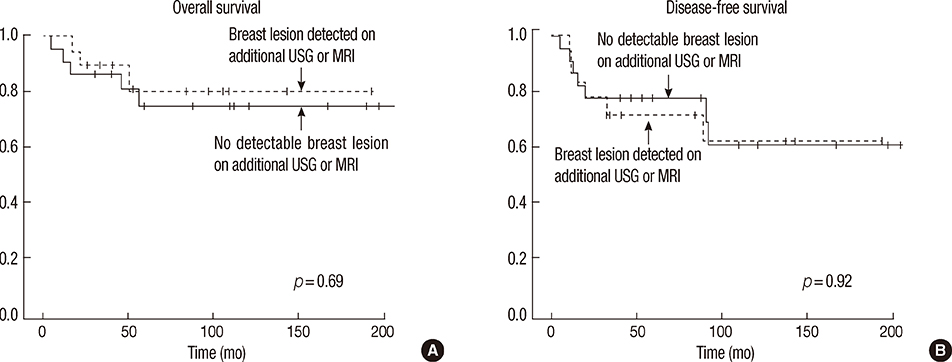
A retrospective study was conducted in which forty OBC patients with axillary lymph node metastasis were identified out of 15,029 patients who had been diagnosed with a primary breast cancer at between 1992 and 2010. The patients were categorized into three treatment groups based on ipsilateral breast management: breast-conserving surgery (BCS) (n=17), mastectomy (n=12), and nonsurgical intervention with or without radiation therapy (No surgery with or without radiation therapy [No Op+/-RT]) (n=11). All patients underwent axillary lymph node dissection. Cases were evaluated based on treatment and potential prognostic factors with respect to overall survival (OS) and disease-free survival (DFS).
RESULTS
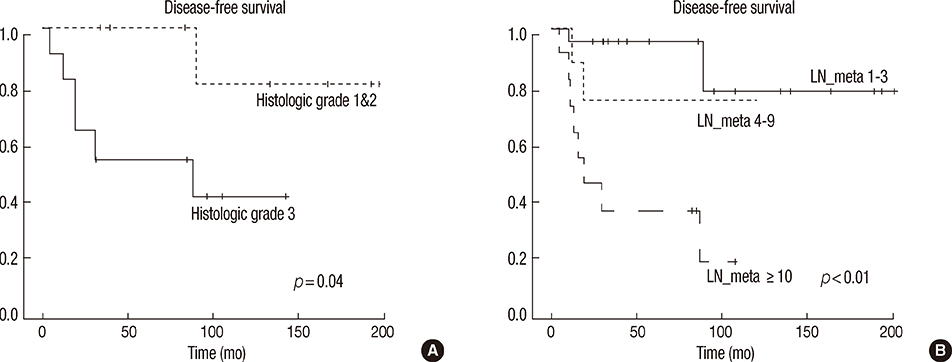
During the follow-up period (median follow-up of 71.5 months), the overall OS and DFS were 76.9% and 74.9%, respectively. The 5-year treatment-specific OS was 72.0% for the BCS group, 74.0% for the mastectomy group, and 87.5% for the No Op+/-RT group (log-rank p=0.49). The 5-year DFS was 70.6% for the BCS group, 66.7% for the mastectomy group, and 90.9% for the No Op+/-RT group (log-rank p=0.36). Recurrence rates for the BCS and No Op+/-RT groups were 5.9% and 18.2%, respectively. Histologic grade and lymph node status were inversely correlated with DFS (log-rank p=0.04 and p<0.01, respectively).
CONCLUSION
There was no difference in survival outcomes between the three treatment methods for the ipsilateral breast (mastectomy, BCS, and No Op+/-RT) of OBC patients with axillary lymph node metastasis. A large-scale multicenter study is needed to validate the results from this small retrospective study.
MeSH Terms
Figure
Reference
-
1. Walker GV, Smith GL, Perkins GH, Oh JL, Woodward W, Yu TK, et al. Population-based analysis of occult primary breast cancer with axillary lymph node metastasis. Cancer. 2010; 116:4000–4006.
Article2. Merson M, Andreola S, Galimberti V, Bufalino R, Marchini S, Veronesi U. Breast carcinoma presenting as axillary metastases without evidence of a primary tumor. Cancer. 1992; 70:504–508.
Article3. van Ooijen B, Bontenbal M, Henzen-Logmans SC, Koper PC. Axillary nodal metastases from an occult primary consistent with breast carcinoma. Br J Surg. 1993; 80:1299–1300.
Article4. Carlson RW, Edge SB, Theriault RL. NCCN Breast Cancer Practice Guidelines Panel. NCCN: breast cancer. Cancer Control. 2001; 8:6 Suppl 2. 54–61.5. Wang X, Zhao Y, Cao X. Clinical benefits of mastectomy on treatment of occult breast carcinoma presenting axillary metastases. Breast J. 2010; 16:32–37.
Article6. Khandelwal AK, Garguilo GA. Therapeutic options for occult breast cancer: a survey of the American Society of Breast Surgeons and review of the literature. Am J Surg. 2005; 190:609–613.
Article7. Buchanan CL, Morris EA, Dorn PL, Borgen PI, Van Zee KJ. Utility of breast magnetic resonance imaging in patients with occult primary breast cancer. Ann Surg Oncol. 2005; 12:1045–1053.
Article8. Olson JA Jr, Morris EA, Van Zee KJ, Linehan DC, Borgen PI. Magnetic resonance imaging facilitates breast conservation for occult breast cancer. Ann Surg Oncol. 2000; 7:411–415.
Article9. Chan SW, Cheung PS, Chan S, Lau SS, Wong TT, Ma M, et al. Benefit of ultrasonography in the detection of clinically and mammographically occult breast cancer. World J Surg. 2008; 32:2593–2598.
Article10. Ahn SH, Park JM, Gong G. Axillary lymph node presentation with occult breast carcinoma. J Korean Surg Soc. 1998; 54:482–487.11. Foroudi F, Tiver KW. Occult breast carcinoma presenting as axillary metastases. Int J Radiat Oncol Biol Phys. 2000; 47:143–147.
Article12. Barton SR, Smith IE, Kirby AM, Ashley S, Walsh G, Parton M. The role of ipsilateral breast radiotherapy in management of occult primary breast cancer presenting as axillary lymphadenopathy. Eur J Cancer. 2011; 47:2099–2106.
Article13. Vlastos G, Jean ME, Mirza AN, Mirza NQ, Kuerer HM, Ames FC, et al. Feasibility of breast preservation in the treatment of occult primary carcinoma presenting with axillary metastases. Ann Surg Oncol. 2001; 8:425–431.
Article14. Kemeny MM, Rivera DE, Terz JJ, Benfield JR. Occult primary adenocarcinoma with axillary metastases. Am J Surg. 1986; 152:43–47.
Article15. Baron PL, Moore MP, Kinne DW, Candela FC, Osborne MP, Petrek JA. Occult breast cancer presenting with axillary metastases. Updated management. Arch Surg. 1990; 125:210–214.
Article16. Vilcoq JR, Calle R, Ferme F, Veith F. Conservative treatment of axillary adenopathy due to probable subclinical breast cancer. Arch Surg. 1982; 117:1136–1138.
Article17. Lee WJ, Chu JS, Chang KJ, Chen KM. Occult breast carcinoma: use of color Doppler in localization. Breast Cancer Res Treat. 1996; 37:299–302.18. Campana F, Fourquet A, Ashby MA, Sastre X, Jullien D, Schlienger P, et al. Presentation of axillary lymphadenopathy without detectable breast primary (T0 N1b breast cancer): experience at Institut Curie. Radiother Oncol. 1989; 15:321–325.
Article19. He M, Tang LC, Yu KD, Cao AY, Shen ZZ, Shao ZM, et al. Treatment outcomes and unfavorable prognostic factors in patients with occult breast cancer. Eur J Surg Oncol. 2012; 38:1022–1028.
Article20. Halsted WS. I. The results of radical operations for the cure of carcinoma of the breast. Ann Surg. 1907; 46:1–19.
Article21. El-Bastawissi AY, White E, Mandelson MT, Taplin S. Variation in mammographic breast density by race. Ann Epidemiol. 2001; 11:257–263.
Article22. del Carmen MG, Halpern EF, Kopans DB, Moy B, Moore RH, Goss PE, et al. Mammographic breast density and race. AJR Am J Roentgenol. 2007; 188:1147–1150.
Article23. Lee CH, Dershaw DD, Kopans D, Evans P, Monsees B, Monticciolo D, et al. Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J Am Coll Radiol. 2010; 7:18–27.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ipsilateral Breast Tumor Recurrence with Metachronous Contralateral Axillary Lymph Node Metastasis after Breast-Conserving Surgery with Axillary Lymph Node Dissection
- Occult Breast Cancers Manifesting as Axillary Lymph Node Metastasis in Men: A Two-Case Report
- Sentinel Lymph Node Biopsy in Breast Cancer Patients With Pathological Complete Response in the Axillary Lymph Node After Neoadjuvant Chemotherapy
- Ultrasonography for Staging Axillary Lymph Node in Breast Cancer Patients
- Axillary sparganosis which was misunderstood lymph node metastasis during neoadjuvant chemotheraphy in a breast cancer patient