J Korean Med Sci.
2012 Jan;27(1):40-45. 10.3346/jkms.2012.27.1.40.
Optimal Baseline Prostate-Specific Antigen Level to Distinguish Risk of Prostate Cancer in Healthy Men Between 40 and 69 Years of Age
- Affiliations
-
- 1Department of Urology, Yongin Severance Hospital, Yonsei University Health System, Yongin, Korea.
- 2Department of Urology, Gangnam Severance Hospital, Yonsei University Health System, Seoul, Korea. chung646@yuhs.ac
- 3Department of Urology, Severance Hospital, Yonsei University Health System, Seoul, Korea.
- KMID: 1792977
- DOI: http://doi.org/10.3346/jkms.2012.27.1.40
Abstract
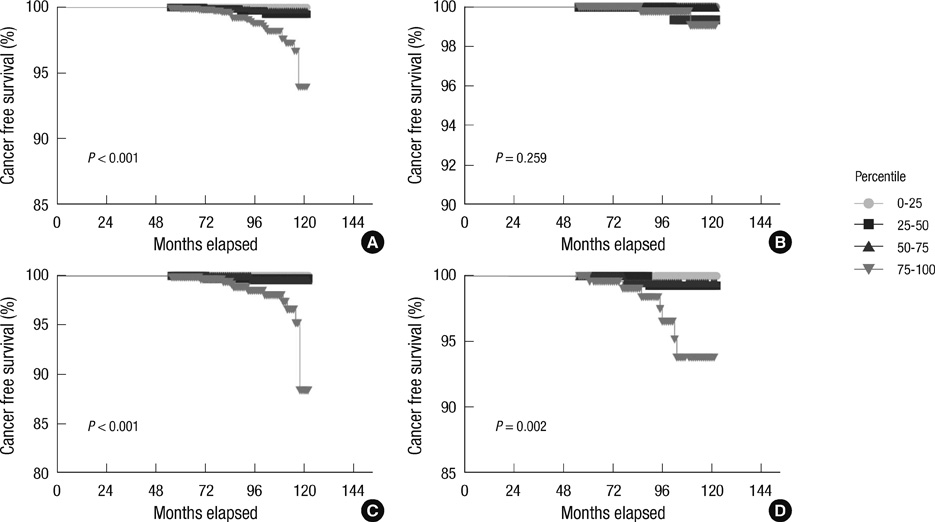
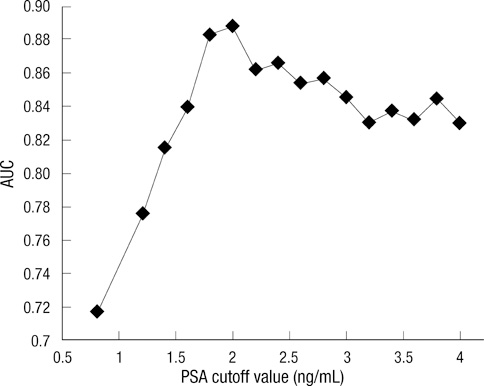
- The present study evaluated optimal baseline prostate-specific antigen (PSA) level at different ages in order to determine the risk of developing prostate cancer (CaP). We analyzed 6,651 Korean men, aged 40-69 yr. The serum PSA levels for these men were measured at one institute from 2000 to 2004 and were determined to be between 0-4 ng/mL. Patients were divided into 4 groups of 25th-percentile intervals, based on initial PSA level. Of these, the group with an increased risk was selected, and the optimal value was determined by the maximal area under a receiver-operating characteristic curve within the selected group. The risk of CaP diagnosis was evaluated by Cox regression. The mean follow-up period was 8.3 yr. CaP was detected in 27 of the 6,651 subjects. CaP detection rate was increased according to age. The optimal PSA value to distinguish the risk of CaP was 2.0 ng/mL for 50- to 69-yr-olds. Patients with a baseline PSA level greater than the optimal value had a 27.78 fold increase in the prostate cancer risk. Baseline PSA values are useful for determining the risk of developing CaP in Korean men for 50- and 69-yr-old. We suggest that PSA testing intervals be modified based on their baseline PSA levels.
MeSH Terms
Figure
Reference
-
1. Wolf AM, Wender RC, Etzioni RB, Thompson IM, D'Amico AV, Volk RJ, Brooks DD, Dash C, Guessous I, Andrews K, DeSantis C, Smith RA. American Cancer Society Prostate Cancer Advisory Committee. American Cancer Society guideline for the early detection of prostate cancer: update 2010. CA Cancer J Clin. 2010. 60:70–98.2. Greene KL, Albertsen PC, Babaian RJ, Carter HB, Gann PH, Han M, Kuban DA, Sartor AO, Stanford JL, Zietman A, Carroll P. Prostate specific antigen best practice statement: 2009 update. J Urol. 2009. 182:2232–2241.3. Whittemore AS, Cirillo PM, Feldman D, Cohn BA. Prostate specific antigen levels in young adulthood predict prostate cancer risk: results from a cohort of Black and White Americans. J Urol. 2005. 174:872–876.4. Loeb S, Roehl KA, Antenor JA, Catalona WJ, Suarez BK, Nadler RB. Baseline prostate-specific antigen compared with median prostate-specific antigen for age group as predictor of prostate cancer risk in men younger than 60 years old. Urology. 2006. 67:316–320.5. Choi YD, Kang DR, Nam CM, Kim YS, Cho SY, Kim SJ, Cho IR, Cho JS, Hong SJ, Ham WS. Age-specific prostate-specific antigen reference ranges in Korean men. Urology. 2007. 70:1113–1116.6. Ku JH, Ahn JO, Lee CH, Lee NK, Park YH, Byun SS, Kwak C, Lee SE. Distribution of serum prostate-specific antigen in healthy Korean men: influence of ethnicity. Urology. 2002. 60:475–479.7. Lee SE, Kwak C, Park MS, Lee CH, Kang W, Oh SJ. Ethnic differences in the age-related distribution of serum prostate-specific antigen values: a study in a healthy Korean male population. Urology. 2000. 56:1007–1010.8. Ahn YO. Cancer registration in Korea: the present and furtherance. J Prev Med Public Health. 2007. 40:265–272.9. Loeb S, Carter HB, Catalona WJ, Moul JW, Schroder FH. Baseline prostate-specific antigen testing at a young age. Eur Urol. 2012. 61:1–7.10. Crawford ED, Moul JW, Rove KO, Pettaway CA, Lamerato LE, Hughes A. Prostate-specific antigen 1.5-4.0 ng/mL: a diagnostic challenge and danger zone. BJU Int. 2011. 108:1743–1749.11. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005. 55:74–108.12. Fang J, Metter EJ, Landis P, Chan DW, Morrell CH, Carter HB. Low levels of prostate-specific antigen predict long-term risk of prostate cancer: results from the Baltimore Longitudinal Study of Aging. Urology. 2001. 58:411–416.13. Loeb S, Nadler RB, Roehl KA, Antenor JA, Catalona WJ. Risk of prostate cancer for young men with a prostate specific antigen less than their age specific median. J Urol. 2007. 177:1745–1748.14. Tang P, Sun L, Uhlman MA, Robertson CN, Polascik TJ, Albala DM, Donatucci CF, Moul JW. Initial prostate specific antigen 1.5 ng/mL or greater in men 50 years old or younger predicts higher prostate cancer risk. J Urol. 2010. 183:946–950.15. Schröder FH, Raaijmakers R, Postma R, van der Kwast TH, Roobol MJ. 4-year prostate specific antigen progression and diagnosis of prostate cancer in the European Randomized Study of Screening for Prostate Cancer, section Rotterdam. J Urol. 2005. 174:489–494.16. Ito K, Raaijmakers R, Roobol M, Wildhagen M, Yamanaka H, Schröder FH. Prostate carcinoma detection and increased prostate-specific antigen levels after 4 years in Dutch and Japanese males who had no evidence of disease at initial screening. Cancer. 2005. 103:242–250.17. Wright EJ, Fang J, Metter EJ, Partin AW, Landis P, Chan DW, Carter HB. Prostate specific antigen predicts the long-term risk of prostate enlargement: results from the Baltimore Longitudinal Study of Aging. J Urol. 2002. 167:2484–2487.18. National Cancer Institute, Division of Cancer Control and Population Science, Surveillance Research Program, Cancer statistics Branch, Surveilance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: mortality-all cause of death, public-use with state, Total U.S. (1969-2007), Underlying mortality data provided by National Center for Health Statistics. 2007.19. Korea National Statistics Office. The Statistics Korea: annual report on the cause of death statistics (based on vital registration). 2007. Daejeon: Korea National Statistics Office.20. Jung KW, Park S, Kong HJ, Won YJ, Boo YK, Shin HR, Park EC, Lee JS. Cancer statistics in Korea: incidence, mortality and survival in 2006-2007. J Korean Med Sci. 2010. 25:1113–1121.21. Antenor JA, Han M, Roehl KA, Nadler RB, Catalona WJ. Relationship between initial prostate specific antigen level and subsequent prostate cancer detection in a longitudinal screening study. J Urol. 2004. 172:90–93.22. Yamamoto T, Ito K, Ohi M, Kubota Y, Suzuki K, Fukabori Y, Kurokawa K, Yamanaka H. Diagnostic significance of digital rectal examination and transrectal ultrasonography in men with prostate-specific antigen levels of 4 NG/ML or less. Urology. 2001. 58:994–998.23. Carvalhal GF, Smith DS, Mager DE, Ramos C, Catalona WJ. Digital rectal examination for detecting prostate cancer at prostate specific antigen levels of 4 ng/ml or less. J Urol. 1999. 161:835–839.24. Vis AN, Hoedemaeker RF, Roobol M, van der Kwast TH, Schröder FH. Tumor characteristics in screening for prostate cancer with and without rectal examination as an initial screening test at low PSA (0.0-3.9 ng/mL). Prostate. 2001. 47:252–261.25. Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, Parnes HL, Minasian LM, Ford LG, Lippman SM, Crawford ED, Crowley JJ, Coltman CA Jr. Prevalence of prostate cancer among men with a prostate-specific antigen level < or =4.0 ng per milliliter. N Engl J Med. 2004. 350:2239–2246.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of Prostate Specific Antigen (PSA) Velocity with Age and Initial PSA in Healthy Korean Men
- Significance of Serum Testosterone for Prostate-Specific Antigen (PSA) Elevation and Prediction of Prostate Cancer in Patients with PSA Above 10 ng/ml
- The Diagnostic Value of Prostate-specific Antigen and the of Routine Laboratory Examination for Early Detection
- Age-specific Reference Ranges and Cutoff Point of Prostate Specific Antigen in Normal Korean Men
- Reevaluation of the Reference Range of Prostate-specific Antigen in Korean Men