J Korean Acad Nurs.
2014 Aug;44(4):418-427. 10.4040/jkan.2014.44.4.418.
Association between Efficiency and Quality of Health Care in South Korea Long-term Care Hospitals: Using the Data Envelopment Analysis and Matrix Analysis
- Affiliations
-
- 1Department of Public Health Science, Graduate School, Korea University, Seoul, Korea.
- 2BK21Plus Program in Public Health Science, Korea University, Seoul, Korea.
- 3School of Health Policy & Management, College of Public Health Science, Korea University, Seoul, Korea. mkchoi@korea.ac.kr
- KMID: 1791871
- DOI: http://doi.org/10.4040/jkan.2014.44.4.418
Abstract
- PURPOSE
Objectives of this study were to investigate the association between efficiency and quality of health care in Long-term Care Hospitals (LTCH) and determine related factors that would enable achievement of both high efficiency and high quality at the same time.
METHODS
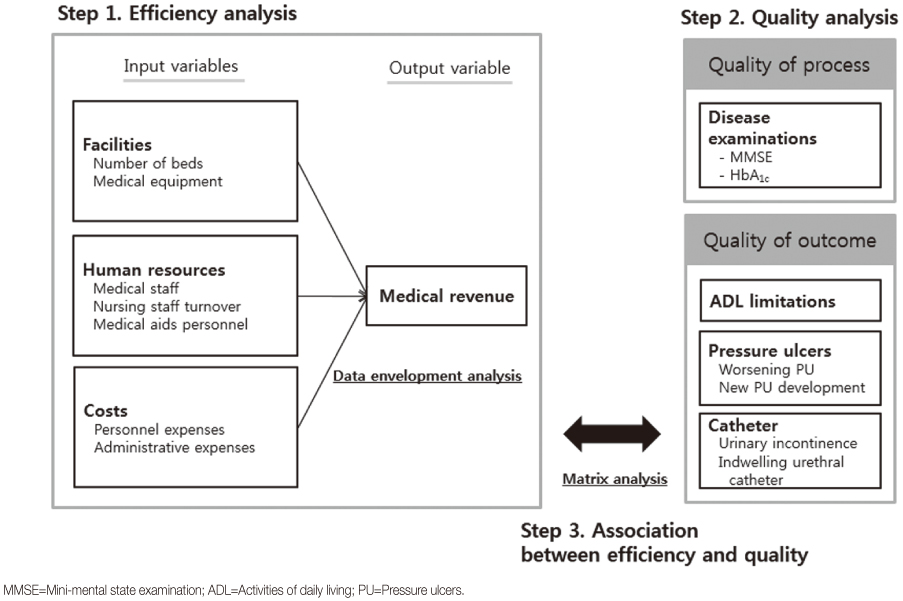
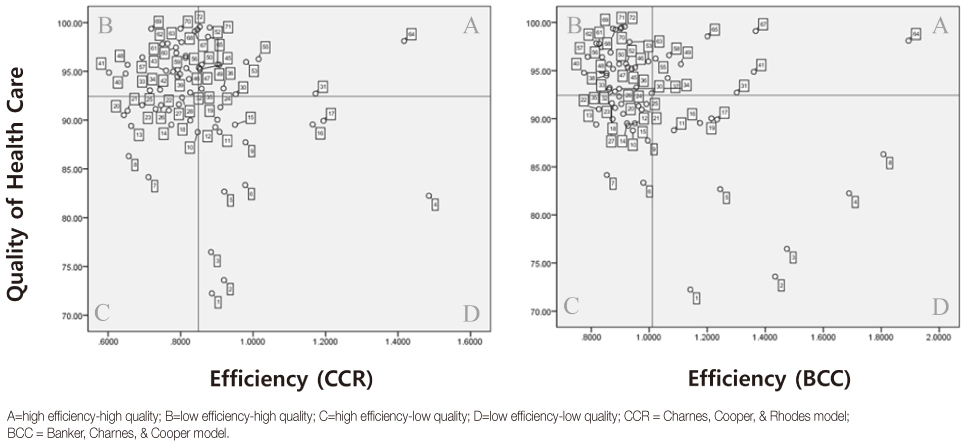
Major data sources were the "2012 Korean Assessment of Propriety by Long-term Care Hospitals" obtained from the Health Insurance Review & Assessment Service. Cost variables were supplemented by a National Tax Service accounting document. First, data envelopment analysis was performed by generating efficiency scores for each LTCH. Second, matrix analysis was conducted to ascertain association between efficiency and quality. Lastly, kruskal-wallis and mann-whitney tests were conducted to identify related factors.
RESULTS
First, efficiency and quality of care are not in a relationship of trade-offs; thus, LTCH can be confident that high efficiency-high quality can be achieved. Second, LTCH with a large number of beds, longer tenure of medical personnel, and adequate levels of investment were more likely to have improved quality as well as efficiency.
CONCLUSION
It is essential to enforce legal standards appropriate to the facilities, reduce turnover of nursing staff, and invest properly in human resources. These consequences will help LTCH to maintain the balance of high efficiency-high quality in the long-run.
MeSH Terms
Figure
Cited by 1 articles
-
Person-centered Care and Nursing Service Quality of Nurses in Long-term Care Hospitals
Hae Sagong, Ga Eon Lee
J Korean Acad Community Health Nurs. 2016;27(4):309-318. doi: 10.12799/jkachn.2016.27.4.309.
Reference
-
1. Statistics Korea. Population projections for Korea: 2010-2060. Daejeon: Author;2011.2. Health Insurance Review & Assessment Service. 2011 national health insurance statistical yearbook. Seoul: Health Insurance Review & Assessment Service, National Health Insurance Service;2012.3. National Health Insurance Service. 2013 evaluation results of longterm care facility. Press Release. 2014. 04. 28.4. The Organisation for Economic Co-operation and Development. OECD health policies and data 2010 [Internet]. Paris, FR: Author;2010. cited 2014 January 20. Available from: http://www.oecd.org/els/health-systems/.5. Health Insurance Review & Assessment Service. Effective management of long-term care hospital. Seoul: Author;2010. 12. Report No.: HETA2000-0139-2824.6. Shimshak DG, Lenard ML, Klimberg RK. Incorporating quality into data envelopment analysis of nursing home performance: A case study. Omega. 2009; 37(3):672–685. http://dx.doi.org/10.1016/j.omega.2008.05.004.7. DeLellis NO, Ozcan YA. Quality outcomes among efficient and inefficient nursing homes: A national study. Health Care Manage Rev. 2013; 38(2):156–165. http://dx.doi.org/10.1097/HMR.0b013e31824bec38.8. Nayar P, Ozcan YA, Yu F, Nguyen AT. Benchmarking urban acute care hospitals: Efficiency and quality perspectives. Health Care Manage Rev. 2013; 38(2):137–145. http://dx.doi.org/10.1097/HMR.0b013e3182527a4c.9. Lee HY, Blegen MA, Harrington C. The effects of RN staffing hours on nursing home quality: A two-stage model. Int J Nurs Stud. 2014; 51(3):409–417. http://dx.doi.org/10.1016/j.ijnurstu.2013.10.007.10. Berta W, Laporte A, Kachan N. Unpacking the relationship between operational efficiency and quality of care in Ontario long-term care homes. Can J Aging. 2010; 29(4):543–556. http://dx.doi.org/10.1017/s0714980810000553.11. Keaysa S, Wistera AV, Gutmana GM. Administrators and quality of care in long-term care facilities. J Hous Elderly. 2009; 23(3):243–260. http://dx.doi.org/10.1080/02763890903035621.12. Rantz MJ, Hicks L, Grando V, Petroski GF, Madsen RW, Mehr DR, et al. Nursing home quality, cost, staffing, and staff mix. Gerontologist. 2004; 44(1):24–38.13. Blank JL, Eggink E. A quality-adjusted cost function in a regulated industry: The case of Dutch nursing homes. Health Care Manag Sci. 2001; 4(3):201–211.14. Anderson RI, Hobbs BK, Weeks HS, Webb JR. Quality of care and nursing home cost-efficiency research. J Real Estate Lit. 2005; 13(3):323–336.15. Lee I, Wang HH. Preliminary development of humanistic care indicators for residents in nursing homes: A delphi technique. Asian Nurs Res. 2014; 8(1):75–81. http://dx.doi.org/10.1016/j.anr.2014.03.001.16. Garavaglia G, Lettieri E, Agasisti T, Lopez S. Efficiency and quality of care in nursing homes: An Italian case study. Health Care Manag Sci. 2011; 14(1):22–35. http://dx.doi.org/10.1007/s10729-010-9139-2.17. Lee RH, Bott MJ, Gajewski B, Taunton RL. Modeling efficiency at the process level: An examination of the care planning process in nursing homes. Health Serv Res. 2009; 44(1):15–32. http://dx.doi.org/10.1111/j.1475-6773.2008.00895.x.18. Duffy JAM, Fitzsimmons JA, Jain N. Identifying and studying "best-performing" services: An application of DEA to long-term care. Benchmarking. 2006; 13(3):232–251. http://dx.doi.org/10.1108/14635770610668767.19. Lee SH. Multi-level analysis of factors related to quality of service in long-term care hospitals. J Korean Acad Nurs. 2009; 39(3):409–421. http://dx.doi.org/10.4040/jkan.2009.39.3.409.20. Cooper WW, Seiford LM, Zhu J. Data envelopment analysis: History, models and interpretations. In : Cooper WW, Seiford LM, Zhu J, editors. Handbook on data envelopment analysis. 2nd ed. New York, NY: Springer;2011. p. 1–39.21. Nayar P, Ozcan YA. Data envelopment analysis comparison of hospital efficiency and quality. J Med Syst. 2008; 32(3):193–199.22. Donabedian A. Quality assessment and assurance: Unity of purpose, diversity of means. Inquiry. 1988; 25(1):173–192.23. Charnes A, Cooper WW, Rhodes E. Measuring the efficiency of decision making units. Eur J Oper Res. 1978; 2(6):429–444. http://dx.doi.org/10.1016/0377-2217(78)90138-8.24. O'Neill L, Rauner M, Heidenberger K, Kraus M. A cross-national comparison and taxonomy of DEA-based hospital efficiency studies. Socioecon Plann Sci. 2008; 42(3):158–189. http://dx.doi.org/10.1016/j.seps.2007.03.001.25. Zhu J. Super-efficiency and DEA sensitivity analysis. Eur J Oper Res. 2001; 129(2):443–455. http://dx.doi.org/10.1016/S0377-2217(99)00433-6.26. Martilla JA, James JC. Importance-performance analysis: An easily-applied technique for measuring attribute importance and performance can further the development of effective marketing programs. J Mark. 1977; 41(1):77–79.27. Zhang NJ, Unruh L, Wan TT. Has the medicare prospective payment system led to increased nursing home efficiency? Health Serv Res. 2008; 43(3):1043–1061. http://dx.doi.org/10.1111/j.1475-6773.2007.00798.x.28. Bostick JE, Rantz MJ, Flesner MK, Riggs CJ. Systematic review of studies of staffing and quality in nursing homes. J Am Med Dir Assoc. 2006; 7(6):366–376. http://dx.doi.org/10.1016/j.jamda.2006.01.024.29. Castle NG, Engberg J. Staff turnover and quality of care in nursing homes. Med Care. 2005; 43(6):616–626.30. Newhouse JP. Toward a theory of nonprofit institutions: An economic model of a hospital. Am Econ Rev. 1970; 60(1):64–74.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Related to Healthcare Service Quality in Long-term Care Hospitals in South Korea: A Mixed-methods Study
- The Performance Evaluation of Public Municipal Hospitals: Data Envelopment Analysis and Panel Analysis
- Improving Service Quality in Long-term Care Hospitals: National Evaluation on Long-term Care Hospitals and Employees Perception of Quality Dimensions
- Key Issues on Long-Term Care Hospitals in Korea
- Multi-level Analysis of Factors related to Quality of Service in Long-term Care Hospitals