Korean J Radiol.
2005 Jun;6(2):94-101. 10.3348/kjr.2005.6.2.94.
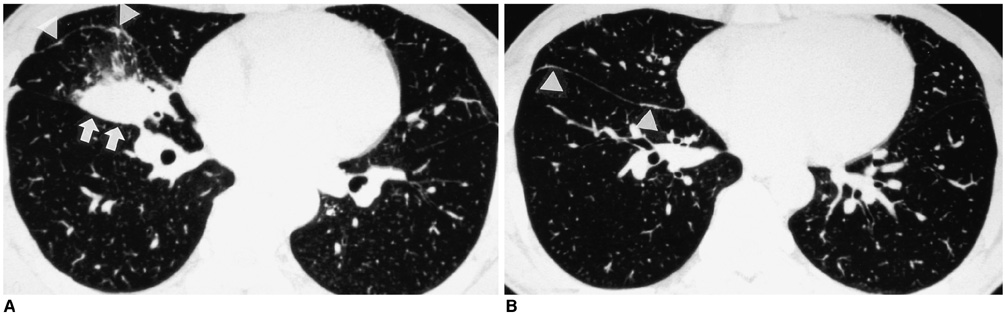
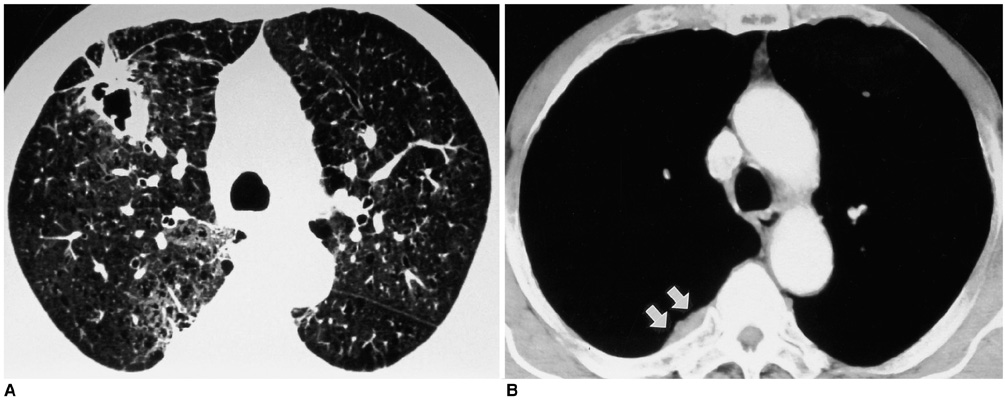
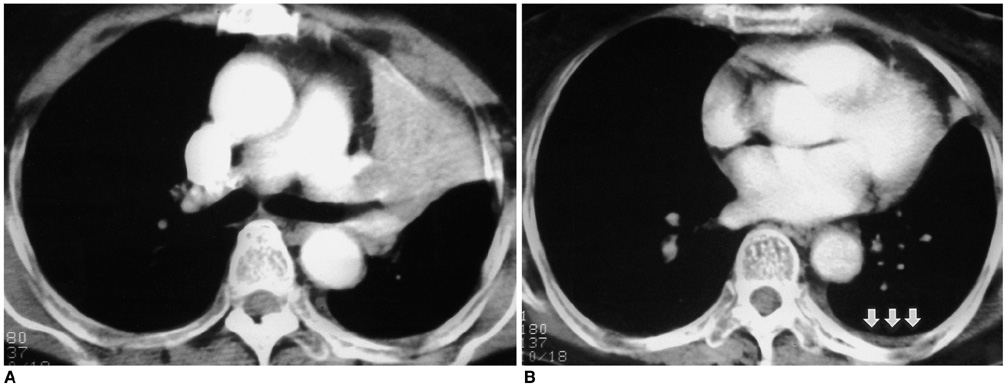
Subtle Pleural Metastasis without Large Effusion in Lung Cancer Patients: Preoperative Detection on CT
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Hospital, Korea. jhhwang@hosp.sch.ac.kr
- 2Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Korea.
- 3Department of Thoracic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Korea.
- KMID: 1783182
- DOI: http://doi.org/10.3348/kjr.2005.6.2.94
Abstract
OBJECTIVE
We wanted to describe the retrospective CT features of subtle pleural metastasis without large effusion that would suggest inoperable lung cancer. MATERIALS AND METHODS: We enrolled 14 patients who had open thoracotomy attempted for lung cancer, but they were proven to be inoperable due to pleural metastasis. Our study also included 20 control patients who were proven as having no pleural metastasis. We retrospectively evaluated the nodularity and thickening of the pleura and the associated pleural effusion on the preoperative chest CT scans. We reviewed the histologic cancer types, the size, shape and location of the lung cancer and the associated mediastinal lymphadenopathy. RESULTS: Subtle pleural nodularity or focal thickening was noted in seven patients (50%) having pleural metastasis and also in three patients (15%) of control group who were without pleural metastasis. More than one of the pleural changes such as subtle pleural nodularity, focal thickening or effusion was identified in eight (57%) patients having pleural metastasis and also in three patients (15%) of the control group, and these findings were significantly less frequent in the control group patients than for the patients with pleural metastasis (p = 0.02). The histologic types of primary lung cancer in patients with pleural metastasis revealed as adenocarcinoma in 10 patients (71%) and squamous cell carcinoma in four patients (29%). The location, size and shape of the primary lung cancer and the associated mediastinal lymphadenopathy showed no significant correlation with pleural metastasis. CONCLUSION: If any subtle pleural nodularity or thickening is found on preoperative chest CT scans of patients with lung cancer, the possibility of pleural metastasis should be considered.
Keyword
MeSH Terms
Figure
Reference
-
1. Kondo H, Asamura H, Suemasu K, Goya T, Tsuchiya R, Naruke T, et al. Prognostic significance of pleural lavage cytology immediately after thoracotomy in patients with lung cancer. J Thorac Cardiovasc Surg. 1993. 106:1092–1097.2. Kjellberg SI, Dresler CM, Goldberg M. Pleural cytologies in lung cancer without pleural effusions. Ann Thorac Surg. 1997. 64:941–944.3. Luh KT, Yang PC, Kuo SH, Chang DB, Yu CJ, Lee LN. Comparison of OK-432 and mitomycin C pleurodesis for malignant pleural effusion caused by lung cancer. A randomized trial. Cancer. 1992. 69:674–679.4. Martini N, Bains MS, Beattie EJ Jr. Indications for pleurectomy in malignant effusion. Cancer. 1975. 35:734–738.5. Moffett MJ, Ruckdeschel JC. Bleomycin and tetracycline in malignant pleural effusions: a review. Semin Oncol. 1992. 19:59–63.6. Hsu CP, Hsu NY, Chen CY. Surgical experience in treating T4 lung cancer: its resectability, morbidity, mortality and prognosis. Eur J Surg Oncol. 1996. 22:171–176.7. Shimizu J, Oda M, Morita K, Hayashi Y, Arano Y, Matsumoto I, et al. Comparison of pleuropneumonectomy and limited surgery for lung cancer with pleural dissemination. J Surg Oncol. 1996. 61:1–6.8. Rodriguez-Panadero F, Borderas Naranjo F, Lopez Mejias J. Pleural metastatic tumours and effusions. Frequency and pathogenic mechanisms in a post-mortem series. Eur Respir J. 1989. 2:366–369.9. Loddenkemper R. Thoracoscopy: results in noncancerous and idiopathic pleural effusions. Poumon-Coeur. 1981. 37:261–264.10. Boutin C, Viallat JR, Cargnino P, Farisse P. Thoracoscopy in malignant pleural effusions. Am Rev Respir Dis. 1981. 124:588–592.11. Willis RA. Willis RA, editor. Transcoelomic metastasis and secondary tumours of the serous membranes. The spread of tumours in the human body. 1973. London: Butterworth;49–60.12. Naidich DP, Muller NL, Zerhouni EA, Webb WR, Krinsky GA. Computed tomography and magnetic resonance of the thorax. 1999. 3rd ed. Philadelphia: Lippincott;349–350.13. Mori K, Hirose T, Machida S, Yokoi K, Tominaga K, Moriyama N, et al. Helical computed tomography diagnosis of pleural dissemination in lung cancer: comparison of thick-section and thin-section helical computed tomography. J Thorac Imaging. 1998. 13:211–218.14. Venuta F, Rendina EA, Ciriaco P, Polettini E, Di Biasi C, Gualdi GF, et al. Computed tomography for preoperative assessment of T3 and T4 bronchogenic carcinoma. Eur J Cardiothorac Surg. 1992. 6:238–241.15. White PG, Adams H, Crane MD, Butchart EG. Preoperative staging of carcinoma of the bronchus: can computed tomographic scanning reliably identify stage III tumors? Thorax. 1994. 49:951–957.16. Murayama S, Murakami J, Yoshimitsu K, Torii Y, Ishida T, Masuda K. CT diagnosis of pleural dissemination without pleural effusion in primary lung cancer. Radiat Med. 1996. 14:117–119.17. Akaogi E, Mitsui K, Onizuka M, Ishikawa S, Tsukada H, Mitsui T. Pleural dissemination in non-small cell lung cancer: results of radiological evaluation and surgical treatment. J Surg Oncol. 1994. 57:33–39.18. Mori M, Mori Y, Mori T, Suzuki A. Computed tomography in the evaluation of pleural dissemination of lung cancer. Lung Cancer. 1988. 28:869–876.19. Yamada K, Ohshita F, Yoshioka T, et al. The early detection of pleural dissemination of lung cancer by thin-slice computed tomography. Lung Cancer. 1995. 35:437–443.20. Eagan RT, Bernatz PE, Payne WS, Pairolero PC, Williams DE, Goellner JR, et al. Pleural lavage after pulmonary resection for bronchogenic carcinoma. J Thorac Cardiovasc Surg. 1984. 88:1000–1003.21. Asamura H, Nakayama H, Kondo H, Tsuchiya R, Naruke T. Thoracoscopic evaluation of histologically/cytologically proven or suspected lung cancer: a VATS exploration. Lung Cancer. 1997. 16:183–190.22. Daniel TM, Kern JA, Tribble CG, Kron IL, Spotnitz WB, Rodgers BM. Thoracoscopic surgery for diseases of the lung and pleura. Effectiveness, changing indications, and limitations. Ann Surg. 1993. 217:566–575.23. Kirby TJ, Mack MJ, Landreneau RJ, Rice TW. Initial experience with video-assisted thoracoscopic lobectomy. Ann Thorac Surg. 1993. 56:1248–1253.24. Roviaro G, Varoli F, Rebuffat C, Vergani C, Maciocco M, Scalambra SM, et al. Videothoracoscopic staging and treatment of lung cancer. Ann Thorac Surg. 1995. 59:971–974.25. Wain JC. Video-assisted thoracoscopy and staging of lung cancer. Ann Thorac Surg. 1993. 56:776–778.26. Lardinois D, Weder W, Hany TF, Kamel EM, Korom S, Seifert B, et al. Staging of non-small-cell lung cancer with integrated positron-emission tomograpy and computed tomography. N Engl J Med. 2003. 348:2500–2507.27. Wahl RL, Quint LE, Greenough RL, Meyer CR, White RI, Orringer MB. Staging of mediastinal non-small cell lung cancer with FDG PET, CT, and fusion images: preliminary prospective evaluation. Radiology. 1994. 191:371–377.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Micro-pleural Metastasis Without Effusion: CT and US Findings
- A Case of a Huge Mass Due to Pleural Metastasis and Management of Dyspnea in a Patient with Terminal Breast Cancer
- Differential CT Features between Malignant Mesothelioma and Pleural Metastasis from Lung Cancer or Extrathoracic Primary Tumor Mimicking Malignant Mesothelioma
- CT Findings of Pleural Dissemination from Lung Cancer
- Distribution of Pleural Effusion Associated with Ascites on Abdominal CT