Korean J Urol.
2009 Aug;50(8):816-818. 10.4111/kju.2009.50.8.816.
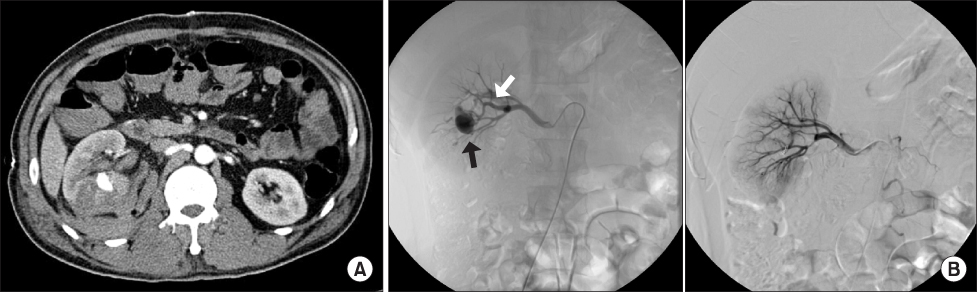
Newly Discovered Pseudoaneurysm after Embolization of a Renal Arteriovenous Fistula with a Pseudoaneurysm following a Renal Stab Wound
- Affiliations
-
- 1Department of Urology, Chonbuk National University Medical School, Institute for Medical Sciences, Jeonju, Korea. sky5115@yahoo.co.kr
- KMID: 1780488
- DOI: http://doi.org/10.4111/kju.2009.50.8.816
Abstract
- Post-traumatic arteriovenous fistula (AVF) and pseudoaneurysm are rare, and mostly occur in stab wound patients. Suspected AVF and pseudoaneurysm requires angiography, with planned simultaneous embolization. Superselective embolization is generally a safe and effective treatment modality for AVF and pseudoaneurysm with minimal associated morbidity. Rare complications of the embolization do occur, including renal abscess, postembolization syndrome, impaired renal function, pulmonary embolism caused by migration of coils, and allergic reaction. We present here the case of a man who presented with a newly discovered pseudoaneurysm after embolization of a renal AVF with pseudoaneurysm after a renal stab wound.
MeSH Terms
Figure
Reference
-
1. Santucci RA, Wessells H, Bartsch G, Descotes J, Heyns CF, McAninch JW, et al. Evaluation and management of renal injuries: consensus statement of the renal trauma subcommittee. BJU Int. 2004. 93:937–954.2. Brandes SB, McAninch JW. Taneja SS, Smith RB, Ehrlich RM, editors. Complications of renal trauma. Complications of urology. 2001. 3rd ed. Philadelphia: Saunders;205–225.3. Bernath AS, Schutte H, Fernandez RR, Addonizio JC. Stab wounds of the kidney: conservative management in flank penetration. J Urol. 1983. 129:468–470.4. Kansas BT, Eddy MJ, Mydlo JH, Uzzo RG. Incidence and management of penetrating renal trauma in patients with multiorgan injury: extended experience at an inner city trauma center. J Urol. 2004. 172:1355–1360.5. Armenakas NA, Duckett CP, McAninch JW. Indications for nonoperative management of renal stab wounds. J Urol. 1999. 161:768–771.6. Benson DA, Stockinger ZT, McSwain NE Jr. Embolization of an acute renal arteriovenous fistula following a stab wound: case report and review of the literature. Am Surg. 2005. 71:62–65.7. Kim HS, Ryu SB, Min BK. A case of control of renal hemorrhage by selective renal arterial embolization. Korean J Urol. 1988. 29:324–328.8. Hwang HH, Cheon SH, Moon KH, Lee SK, Choo HS, Hwang JC, et al. Renal ruptures with active bleeding treated with emergency selective renal arterial embolizaton. Korean J Urol. 2008. 49:177–181.9. Heyns CF, Van Vollenhoven P. Selective surgical management of renal stab wounds. Br J Urol. 1992. 69:351–357.10. Al-Qudah HS, Santucci RA. Complications of renal trauma. Urol Clin North Am. 2006. 33:41–53.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pseudoaneurysm after Renal Biopsy; Angigraphic Diagnosis and Treatment by Superselective Embolization
- A Case of Congenital Renal Arteriovenous Fistula
- Successfully treated isolated renal artery pseudoaneurysm in a patient with Behçet's disease
- Transcatheter arterial embolization for congenital renal arteriovenous fistula
- Endovascular Treatment of a Traumatic Carotid-Jugular Fistula by Using Stent-Graft