Korean J Pain.
2012 Apr;25(2):94-98. 10.3344/kjp.2012.25.2.94.
Effect of Intravenous Lidocaine on the Neuropathic Pain of Failed Back Surgery Syndrome
- Affiliations
-
- 1Department Anesthesiology and Pain Medicine, Daegu Wooridul Spine Hospital, Daegu, Korea. magary1@hanmail.net
- KMID: 1778992
- DOI: http://doi.org/10.3344/kjp.2012.25.2.94
Abstract
- BACKGROUND
An intravenous infusion of lidocaine has been used on numerous occasions to produce analgesia in neuropathic pain. In the cases of failed back surgery syndrom, the pain generated as result of abnormal impulse from the dorsal root ganglion and spinal cord, for instance as a result of nerve injury may be particularly sensitive to lidocaine. The aim of the present study was to identify the effects of IV lidocaine on neuropathic pain items of FBSS.
METHODS
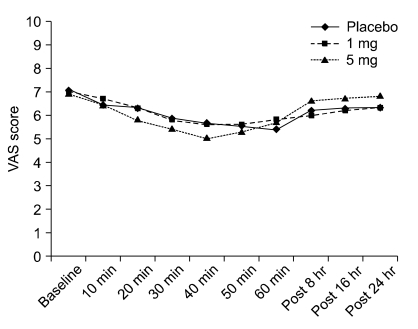
The study was a randomized, prospective, double-blinded, crossover study involving eighteen patients with failed back surgery syndrome. The treatments were: 0.9% normal saline, lidocaine 1 mg/kg in 500 ml normal saline, and lidocaine 5 mg/kg in 500 ml normal saline over 60 minutes. The patients underwent infusions on three different appointments, at least two weeks apart. Thus all patients received all 3 treatments. Pain measurement was taken by visual analogue scale (VAS), and neuropathic pain questionnaire.
RESULTS
Both lidocaine (1 mg/kg, 5 mg/kg) and placebo significantly reduced the intense, sharp, hot, dull, cold, sensitivity, itchy, unpleasant, deep and superficial of pain. The amount of change was not significantly different among either of the lidocaine and placebo, or among the lidocaine treatments themselves, for any of the pain responses, except sharp, dull, cold, unpleasant, and deep pain. And VAS was decreased during infusion in all 3 group and there were no difference among groups.
CONCLUSIONS
This study shows that 1 mg/kg, or 5 mg/kg of IV lidocaine, and palcebo was effective in patients with neuropathic pain attributable to FBSS, but effect of licoaine did not differ from placebo saline.
MeSH Terms
Figure
Reference
-
2. Waguespack A, Schofferman J, Slosar P, Reynolds J. Etiology of long-term failures of lumbar spine surgery. Pain Med. 2002; 3:18–22. PMID: 15102214.
Article3. Burton CV, Kirkaldy-Willis WH, Yong-Hing K, Heithoff KB. Causes of failure of surgery on the lumbar spine. Clin Orthop Relat Res. 1981; 157:191–199. PMID: 7249453.
Article4. Dworkin RH, O'Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010; 85:S3–S14. PMID: 20194146.
Article5. Tremont-Lukats IW, Challapalli V, McNicol ED, Lau J, Carr DB. Systemic administration of local anesthetics to relieve neuropathic pain: a systematic review and meta-analysis. Anesth Analg. 2005; 101:1738–1749. PMID: 16301253.
Article6. Attal N, Gaudé V, Brasseur L, Dupuy M, Guirimand F, Parker F, et al. Intravenous lidocaine in central pain: a double-blind, placebo-controlled, psychophysical study. Neurology. 2000; 54:564–574. PMID: 10680784.
Article7. Baranowski AP, De Courcey J, Bonello E. A trial of intravenous lidocaine on the pain and allodynia of postherpetic neuralgia. J Pain Symptom Manage. 1999; 17:429–433. PMID: 10388248.
Article8. Tanelian DL, MacIver MB. Analgesic concentrations of lidocaine suppress tonic A-delta and C fiber discharges produced by acute injury. Anesthesiology. 1991; 74:934–936. PMID: 2021210.
Article9. Chabal C, Russell LC, Burchiel KJ. The effect of intravenous lidocaine, tocainide, and mexiletine on spontaneously active fibers originating in rat sciatic neuromas. Pain. 1989; 38:333–338. PMID: 2510116.
Article10. Woolf CJ, Wiesenfeld-Hallin Z. The systemic administration of local anaesthetics produces a selective depression of C-afferent fibre evoked activity in the spinal cord. Pain. 1985; 23:361–374. PMID: 3937116.
Article11. Nagy I, Woolf CJ. Lignocaine selectively reduces C fibre-evoked neuronal activity in rat spinal cord in vitro by decreasing N-methyl-D-aspartate and neurokinin receptor-mediated post-synaptic depolarizations; implications for the development of novel centrally acting analgesics. Pain. 1996; 64:59–70. PMID: 8867247.
Article12. Jensen MP. Using pain quality assessment measures for selecting analgesic agents. Clin J Pain. 2006; 22:S9–S13. PMID: 16344610.
Article13. Carroll IR, Younger JW, Mackey SC. Pain quality predicts lidocaine analgesia among patients with suspected neuropathic pain. Pain Med. 2010; 11:617–621. PMID: 20210867.
Article14. Jensen MP, Dworkin RH, Gammaitoni AR, Olaleye DO, Oleka N, Galer BS. Assessment of pain quality in chronic neuropathic and nociceptive pain clinical trials with the Neuropathic Pain Scale. J Pain. 2005; 6:98–106. PMID: 15694876.
Article15. Tremont-Lukats IW, Hutson PR, Backonja MM. A randomized, double-masked, placebo-controlled pilot trial of extended IV lidocaine infusion for relief of ongoing neuropathic pain. Clin J Pain. 2006; 22:266–271. PMID: 16514327.
Article16. Ellemann K, Sjögren P, Banning AM, Jensen TS, Smith T, Geertsen P. Trial of intravenous lidocaine on painful neuropathy in cancer patients. Clin J Pain. 1989; 5:291–294. PMID: 2520418.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Neuropathic Back Pain : Are There Any Practical Diagnostic Criteria?
- The Effect of Psoas Compartment Block for the Relief of Low Lumbar and Both Thigh Pain: A case report
- Intramuscular Stimulation Therapy in Failed Back Surgery Syndrome Patients
- Spinal anesthesia for implantation of a spinal cord stimulator in a patient with failed back surgery syndrome: A case report
- Raiofrequency Neurotomy for Lumbar Facet Joint Pain in the Patients with Failed Back Surgery Syndrome