Korean J Ophthalmol.
2013 Aug;27(4):282-287. 10.3341/kjo.2013.27.4.282.
Effect of Electrocauterization on the Inflammation of the Conjunctiva in Experimental Animal Model
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. kmk9@snu.ac.kr
- 2Laboratory of Corneal Regenerative Medicine and Ocular Immunology, Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- KMID: 1705425
- DOI: http://doi.org/10.3341/kjo.2013.27.4.282
Abstract
- PURPOSE
Recently, conjunctivochalasis repair surgery using electrocauterization has been gaining popularity. However, patients with electrocauterized conjunctivoplasty tend to complain of more postoperative pain than patients undergoing simple excision with suturing. Therefore, we investigated the effects of electrocauterization on inflammation of the conjunctiva using an experimental animal model and compared these with the effects of simple excision with suturing.
METHODS
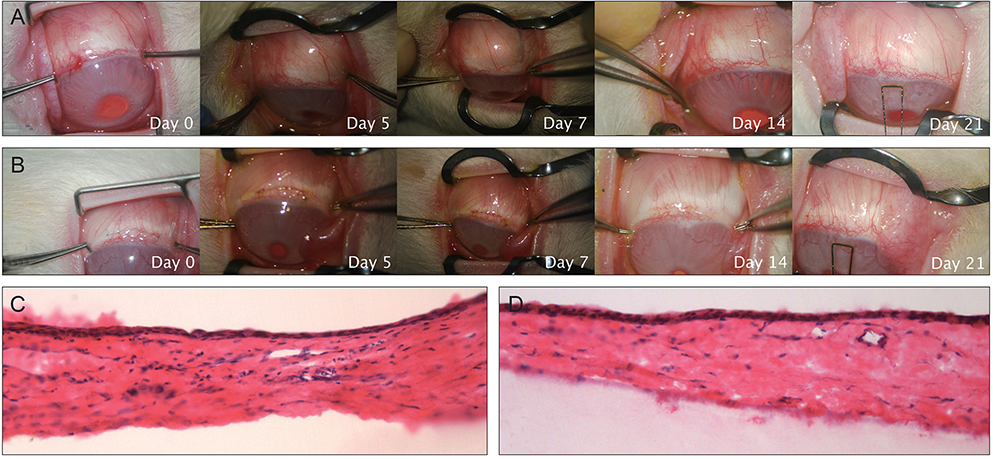
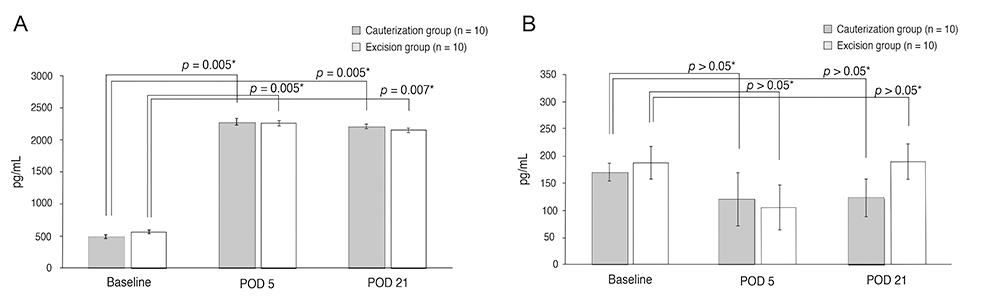
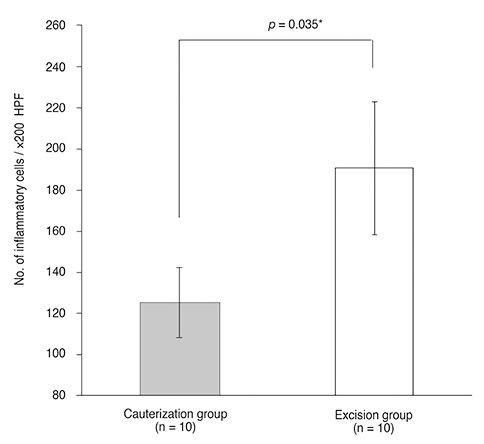
Ten New Zealand white rabbits underwent cauterization in the right eyes and excision and suturing in the left eyes. For each eye, we excised or electrocauterized the inferior bulbar conjunctiva, 1 mm in width and 6 mm in length, 2 mm from the limbus. A fine-needle electrode was inserted subconjunctivally, and electrocauterization was performed. In the contralateral eye, the corresponding area was excised and re-approximated with 10-0 nylon sutures. Sutures were removed after 14 days. Tissue samples were obtained at 21 days post-procedure, and inflammatory cells were counted in five randomly selected fields (x200) on hematoxylin-eosin stained slides. Tumor necrosis factor (TNF)-alpha and interleukin (IL)-1beta concentrations in tears were measured using enzyme linked immunosorbent assays.
RESULTS
All cauterized eyes demonstrated smooth surface healing without scarring after 5 days, whereas sutured eyes presented with mild edema with some scarring until the suture was removed. The number of inflammatory cells was significantly greater in sutured eyes compared with cauterized eyes (p = 0.035, Mann-Whitney U-test) at 21 days post-procedure. Tear TNF-alpha and IL-1beta concentrations at 21 days were similar in both groups.
CONCLUSIONS
Electrocauterization for conjunctivoplasty seems to be advantageous in terms of inflammation compared with simple suturing and excision.
Keyword
MeSH Terms
Figure
Reference
-
1. Hughes WL. Conjunctivochalasis. Am J Ophthalmol. 1942; 25:48–51.2. Liu D. Conjunctivochalasis: a cause of tearing and its management. Ophthal Plast Reconstr Surg. 1986; 2:25–28.3. Meller D, Tseng SC. Conjunctivochalasis: literature review and possible pathophysiology. Surv Ophthalmol. 1998; 43:225–232.4. Jordan DR, Pelletier CR. Conjunctivochalasis. Can J Ophthalmol. 1996; 31:192–193.5. Kheirkhah A, Casas V, Blanco G, et al. Amniotic membrane transplantation with fibrin glue for conjunctivochalasis. Am J Ophthalmol. 2007; 144:311–313.6. Meller D, Maskin SL, Pires RT, Tseng SC. Amniotic membrane transplantation for symptomatic conjunctivochalasis refractory to medical treatments. Cornea. 2000; 19:796–803.7. Otaka I, Kyu N. A new surgical technique for management of conjunctivochalasis. Am J Ophthalmol. 2000; 129:385–387.8. Haefliger IO, Vysniauskiene I, Figueiredo AR, Piffaretti JM. Superficial conjunctiva cauterization to reduce moderate conjunctivochalasis. Klin Monbl Augenheilkd. 2007; 224:237–239.9. Youm DJ, Kim JM, Choi CY. Simple surgical approach with high-frequency radio-wave electrosurgery for conjunctivochalasis. Ophthalmology. 2010; 117:2129–2133.10. Huang SK. Advances in applications of radiofrequency current to catheter ablation therapy. Pacing Clin Electrophysiol. 1991; 14:28–42.11. Hurwitz JJ, Johnson D, Howarth D, Molgat YM. Experimental treatment of eyelashes with high-frequency radio wave electrosurgery. Can J Ophthalmol. 1993; 28:62–64.12. Shoji J, Kawaguchi A, Gotoh A, et al. Concentration of soluble interleukin-6 receptors in tears of allergic conjunctival disease patients. Jpn J Ophthalmol. 2007; 51:332–337.13. Uchino E, Sonoda S, Kinukawa N, Sakamoto T. Alteration pattern of tear cytokines d uring the course of a day: diurnal rhythm analyzed by multicytokine assay. Cytokine. 2006; 33:36–40.14. Stahl JL, Cook EB, Graziano FM, Barney NP. Differential and cooperative effects of TNF-alpha, IL-1beta, and IFN-gamma on human conjunctival epithelial cell receptor expression and chemokine release. Invest Ophthalmol Vis Sci. 2003; 44:2010–2015.15. Leonardi A, Jose PJ, Zhan H, Calder VL. Tear and mucus eotaxin-1 and eotaxin-2 in allergic keratoconjunctivitis. Ophthalmology. 2003; 110:487–492.16. Acera A, Rocha G, Vecino E, et al. Inflammatory markers in the tears of patients with ocular surface disease. Ophthalmic Res. 2008; 40:315–321.17. Solomon A, Dursun D, Liu Z, et al. Pro- and anti-inflammatory forms of interleukin-1 in the tear fluid and conjunctiva of patients with dry-eye disease. Invest Ophthalmol Vis Sci. 2001; 42:2283–2292.18. Nakamura Y, Sotozono C, Kinoshita S. Inflammatory cytokines in normal human tears. Curr Eye Res. 1998; 17:673–676.19. Wilson SE, Mohan RR, Mohan RR, et al. The corneal wound healing response: cytokine-mediated interaction of the epithelium, stroma, and inflammatory cells. Prog Retin Eye Res. 2001; 20:625–637.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Subconjunctival Injection of Bevacizumab After Resection of Muscle in Rabbit Models
- Effect of Electrocauterization on Corneal Astigmatism in Temporal Incision Cataract Surgery
- A Precipitating factor of Acute Gouty Inflammation in an Animal Model and its Histologic contribution
- Experimental Models of Depression
- Treatment of Recurrent Conjunctival Papilloma with Topical Mitomycin C