Korean J Hepatobiliary Pancreat Surg.
2013 Aug;17(3):113-117. 10.14701/kjhbps.2013.17.3.113.
Prognosis of patients with pT1b/T2 gallbladder carcinoma who have undergone laparoscopic cholecystectomy as an initial operation
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 1472526
- DOI: http://doi.org/10.14701/kjhbps.2013.17.3.113
Abstract
- BACKGROUNDS/AIMS
Laparoscopic cholecystectomy (LC) has become a standard procedure for treatment of benign gallbladder diseases. There has been a small proportion of gallbladder cancer (GBC) which was incidentally found in the gallbladder specimen, and LC has been tried in some patients with faintly suspected GBC. This study intended to analyze the prognosis of patients with pT1b/T2 GBC who have undergone LC and the outcome of extended re-operation.
METHODS
After analyzing the institutional profiles of 500 GBC patients who have undergone surgical resection, we selected 64 patients who underwent LC initially from January 1996 to December 2008 and whose gallbladder pathology was confined to pT1b or pT2 lesions. Of them, 34 patients (53.1%) underwent extended reoperation. Their medical records were reviewed retrospectively.
RESULTS
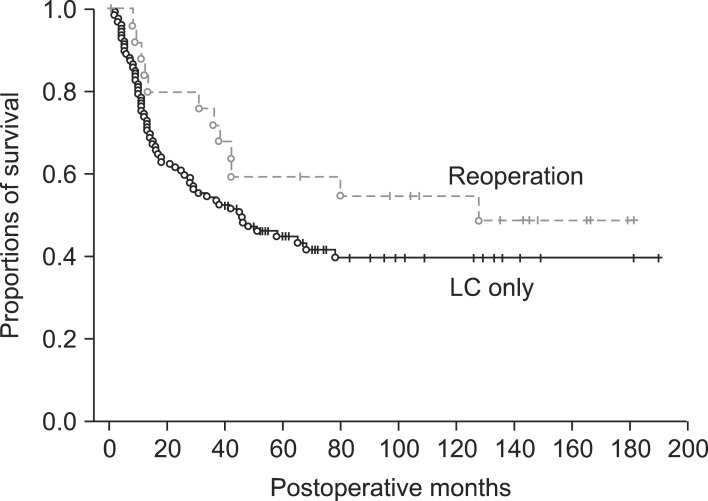
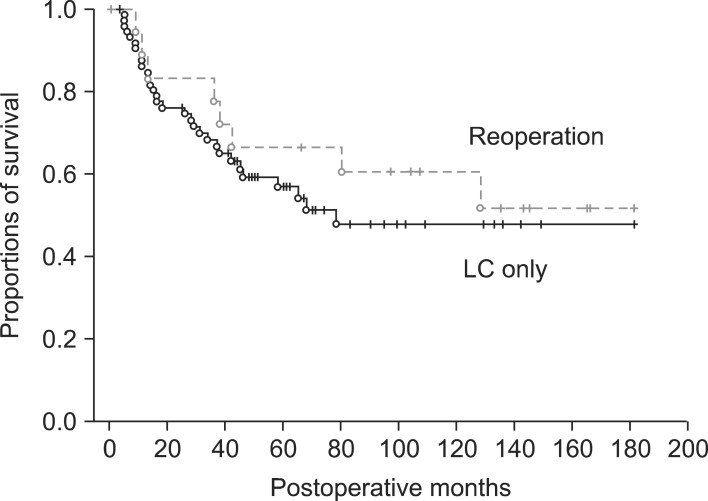
In the LC only group (n=30), mean age of the 16 pT1 patients was 65.7+/-12.5 years and mean age of the 14 pT2 patients was 66.7+/-10.1 years. In the reoperation group (n=34), mean age of the 8 pT1b patients was 52.6+/-9.9 years and in 26 pT2 patients, mean age was 59.2+/-7.9 years. The reoperation group showed a younger patient age pattern than the LC only group (p=0.001). The types of reoperation were liver resection with lymph node (LN) dissection in 17, bile duct resection with LN dissection in 2, and hepatectomy and bile duct resection with LN dissection in 15. In the LC only group, the 5-year survival rate (5-YSR) was 70.3% in pT1b and 43.2% in pT2. In the reoperation group, 5-YSR was 62.5% in pT1b (n=8) and 59.5% in pT2 (n=26). A survival comparison between the two groups showed no significant survival gain in pT1 patients (p=0.69) and in pT2 patients (p=0.14). In our whole database analysis, 5-YSR of pT1bNx lesions was 70% after cholecystectomy and 78% after extended cholecystectomy. Lymph node metastasis was identified in 11% of pT1b lesions. For pT2N0 lesions, overall 5-YSR was 62% after R0 resection, showing no survival difference between primary extended surgery and LC-redo operation (p=0.45).
CONCLUSIONS
The survival gain of reoperation was not evident in pT1b lesions. In contrast, some noticeable but not statistically significant survival difference was observed in pT2 lesions. Thus, reoperation for pT1b/T2 GBC following LC is indicated for individualized reasons, especially in patients with pT1b lesions. Old age was one of the important factors in deciding not to reoperate.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Surgical outcome and prognostic factors in patients with gallbladder carcinoma
Eun Kyung Hong, Kun Kuk Kim, Jung Nam Lee, Woon Kee Lee, Min Chung, Yeon Suk Kim, Yeon Ho Park
Korean J Hepatobiliary Pancreat Surg. 2014;18(4):129-137. doi: 10.14701/kjhbps.2014.18.4.129.
Reference
-
1. Kohya N, Miyazaki K. Hepatectomy of segment 4a and 5 combined with extra-hepatic bile duct resection for T2 and T3 gallbladder carcinoma. J Surg Oncol. 2008; 97:498–502. PMID: 18314875.
Article2. Nimura Y. Extended surgery in bilio-pancreatic cancer: the Japanese experience. Semin Oncol. 2002; 29(6 Suppl 20):17–22. PMID: 12577229.
Article3. Tsukada K, Hatakeyama K, Kurosaki I, et al. Outcome of radical surgery for carcinoma of the gallbladder according to the TNM stage. Surgery. 1996; 120:816–821. PMID: 8909516.
Article4. Ogura Y, Mizumoto R, Isaji S, et al. Radical operations for carcinoma of the gallbladder: present status in Japan. World J Surg. 1991; 15:337–343. PMID: 1853612.
Article5. Sikora SS, Singh RK. Surgical strategies in patients with gallbladder cancer: nihilism to optimism. J Surg Oncol. 2006; 93:670–681. PMID: 16724356.
Article6. Wakai T, Shirai Y, Yokoyama N, et al. Early gallbladder carcinoma does not warrant radical resection. Br J Surg. 2001; 88:675–678. PMID: 11350438.
Article7. Shirai Y, Yoshida K, Tsukada K, et al. Early carcinoma of the gallbladder. Eur J Surg. 1992; 158:545–548. PMID: 1360827.8. Wakai T, Shirai Y, Yokoyama N, et al. Early gallbladder carcinoma does not warrant radical resection. Br J Surg. 2001; 88:675–678. PMID: 11350438.
Article9. de Aretxabala X, Roa I, Burgos L, et al. Gallbladder cancer in Chile. A report on 54 potentially resectable tumors. Cancer. 1992; 69:60–65. PMID: 1727676.
Article10. Ouchi K, Owada Y, Matsuno S, et al. Prognostic factors in the surgical treatment of gallbladder carcinoma. Surgery. 1987; 101:731–737. PMID: 2438791.11. Ogura Y, Mizumoto R, Isaji S, et al. Radical operations for carcinoma of the gallbladder: present status in Japan. World J Surg. 1991; 15:337–343. PMID: 1853612.
Article12. Wagholikar GD, Behari A, Krishnani N, et al. Early gallbladder cancer. J Am Coll Surg. 2002; 194:137–141. PMID: 11848630.
Article13. Wakai T, Shirai Y, Hatakeyama K. Radical second resection provides survival benefit for patients with T2 gallbladder carcinoma first discovered after laparoscopic cholecystectomy. World J Surg. 2002; 26:867–871. PMID: 11960212.
Article14. Toyonaga T, Chijiiwa K, Nakano K, et al. Completion radical surgery after cholecystectomy for accidentally undiagnosed gallbladder carcinoma. World J Surg. 2003; 27:266–271. PMID: 12607049.
Article15. Suzuki S, Yokoi Y, Kurachi K, et al. Appraisal of surgical treatment for pT2 gallbladder carcinomas. World J Surg. 2004; 28:160–165. PMID: 14708053.
Article16. Muratore A, Polastri R, Bouzari H, et al. Radical surgery for gallbladder cancer: a worthwhile operation? Eur J Surg Oncol. 2000; 26:160–163. PMID: 10744936.
Article17. Wakai T, Shirai Y, Yokoyama N, et al. Depth of subserosal invasion predicts long-term survival after resection in patients with T2 gallbladder carcinoma. Ann Surg Oncol. 2003; 10:447–454. PMID: 12734095.
Article18. Shirai Y, Yoshida K, Tsukada K, et al. Inapparent carcinoma of the gallbladder. An appraisal ofa radical second operation after simple cholecystectomy. Ann Surg. 1992; 215:326–331. PMID: 1558412.19. Yamaguchi K, Tsuneyoshi M. Subclinical gallbladder carcinoma. Am J Surg. 1992; 163:382–386. PMID: 1558279.
Article20. Kosuge T, Sano K, Shimada K, et al. Should the bile duct be preserved orremoved in radical surgery for gallbladder cancer? Hepatogastroenterology. 1999; 46:2133–2137. PMID: 10521955.21. Chijiiwa K, Nakano K, Ueda J, et al. Surgical treatment of patients with T2 gallbladder carcinoma invading the subserosal layer. J Am Coll Surg. 2001; 192:600–607. PMID: 11333097.
Article22. Fong Y, Heffernan N, Blumgart LH. Gallbladder carcinoma discovered during laparoscopic cholecystectomy: aggressive reresection is beneficial. Cancer. 1998; 83:423–427. PMID: 9690533.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognosis of Patients with the Gallbladder Carcinoma Undergone Laparoscopic Cholecystectomy as an Initial Operation
- A Case of Squamous Cell Carcinoma of Gallbladder after Laparoscopic Cholecystectomy
- Gallbladder Carcinomas found after a Laparoscopic Cholecystectomy
- What is your initial surgical procedure for suspicious T2 gallbladder cancer? - Minimally invasive surgery.
- Chinical Comparison of the Traditional Versus Laparoscopic Surgery in Cholecystectomy for Cholelithiasis