J Korean Soc Radiol.
2010 Apr;62(4):335-338. 10.3348/jksr.2010.62.4.335.
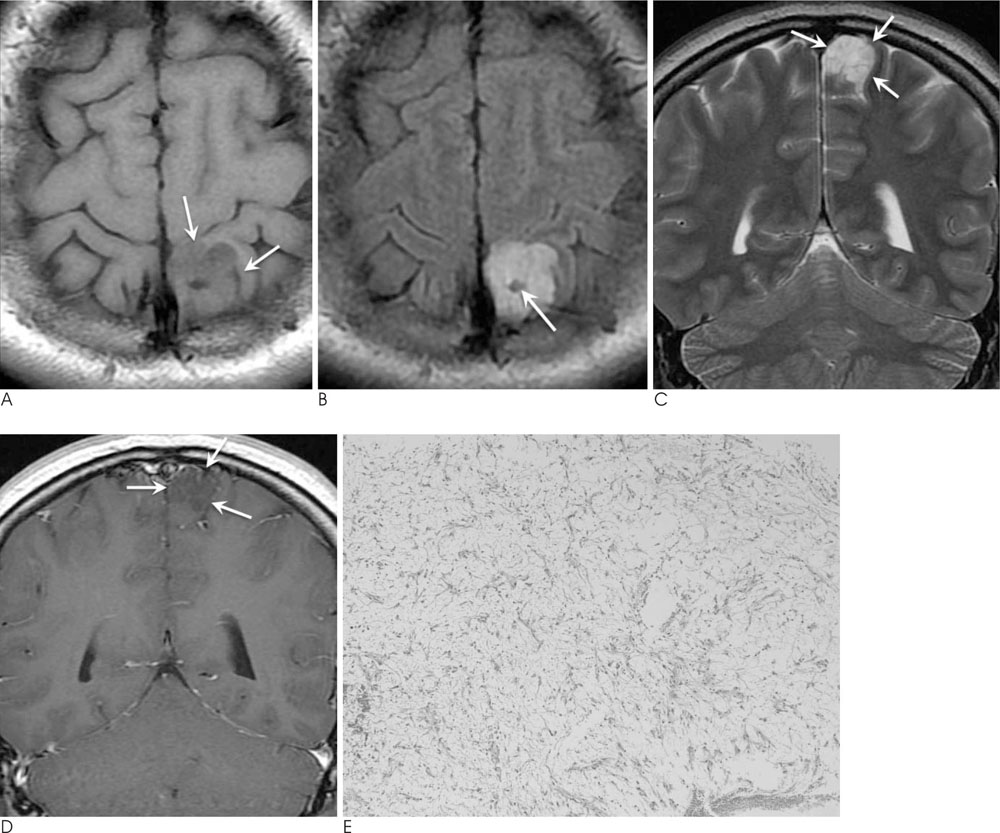
Adult Pilomyxoid Astrocytoma Mimicking a Cortical Brain Tumor: MR Imaging Findings
- Affiliations
-
- 1Department of Radiology, University of Ulsan College of Medicine, Ulsan University Hospital, Korea. ycweon@hanmail.net
- 2Department of Pathology, University of Ulsan College of Medicine, Ulsan University Hospital, Korea.
- 3Department of Neurosurgery, University of Ulsan College of Medicine, Ulsan University Hospital, Korea.
- KMID: 1460064
- DOI: http://doi.org/10.3348/jksr.2010.62.4.335
Abstract
- A pilomyxoid astrocytoma (PMA) is a recently identified low-grade neoplasm that was previously classified as a pilocytic astrocytoma (PA), yet demonstrates unique histological features and more aggressive behavior. Although a PMA is generally a tumor of early childhood and typically occurs in the hypothalamic/chiasmatic region, it can mimic cortical tumors, especially in adults. We report the MR findings of a PMA presenting as a cortical brain tumor in an adult with neurofibromatosis 1 (NF1).
MeSH Terms
Figure
Reference
-
1. Brat DJ, Parisi JE, Kleinschmidt-DeMasters BK, Yachnis AT, Montine TJ, Boyer PJ, et al. Surgical neuropathology update: a review of changes introduced by the WHO classification of tumours of the central nervous system, 4th edition. Arch Pathol Lab Med. 2008; 132:993–1007.2. Tihan T, Fisher PG, Kepner JL, Godfraind C, McComb RD, Goldthwaite PT, et al. Pediatric astrocytomas with monomorphous pilomyxoid features and a less favorable outcome. J Neuropathol Exp Neurol. 1999; 58:1061–1068.3. Komotar RJ, Burger PC, Carson BS, Brem H, Olivi A, Goldthwaite PT, et al. Pilocytic and pilomyxoid hypothalamic/chiasmatic astrocytomas. Neurosurgery. 2004; 54:72–79.4. Linscott LL, Osborn AG, Blaser S, Castillo M, Hewlett RH, Wieselthaler N, et al. Pilomyxoid Astrocytoma: expanding the Imaging Spectrum. AJNR Am J Neuroradiol. 2008; 29:1861–1866.5. Arslanoglu A, Cirak B, Horska A, Okoh J, Tihan T, Aronson L, et al. MR imaging characteristics of pilomyxoid astrocytomas. AJNR Am J Neuroradiol. 2003; 24:1906–1908.6. Komotar RJ, Mocco J, Zacharia BE, Wilson DA, Kim PY, Canoll PD, et al. Astrocytoma with pilomyxoid features presenting in an adult. Neuropathology. 2006; 26:89–93.7. Gottfried ON, Fults DW, Townsend JJ, Couldwell WT. Spontaneous hemorrhage associated with a pilomyxoid astrocytoma: case report. J Neurosurg. 2003; 99:416–420.8. Listernick R, Charrow J, Greenwald M, Mets M. Natural history of optic pathway tumors in children with neurofibromatosis type 1: a longitudinal study. J Pediatr. 1994; 125:63–66.9. Rodriguez FJ, Perry A, Gutmann DH, O'Neill BP, Leonard J, Bryant S, et al. Gliomas in neurofibromatosis type 1: a clinicopathologic study of 100 patients. J Neuropathol Exp Neurol. 2008; 67:240–249.10. Khanani MF, Hawkins C, Shroff M, Dirks P, Capra M, Burger PC, et al. Pilomyxoid astrocytoma in a patient with neurofibromatosis. Pediatr Blood Cancer. 2006; 46:377–380.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Juvenile Pilomyxoid Astrocytoma in the Opticohypothalamus
- Intermediate Pilomyxoid Astrocytoma in the Cerebellum of a 5-Year-Old Boy
- A Case of Anaplastic Astrocytoma in Term Pregnancy
- Intracranial Gossypiboma Mimicking a Recurrent Low Grade Astrocytoma: Case Report
- MR Imaging Findings of Gliosarcoma: Report of Three Cases