J Korean Soc Radiol.
2011 Jul;65(1):61-68. 10.3348/jksr.2011.65.1.61.
Venogram of the Upper Extremity Using the Tourniquet Technique for the Evaluation of Central Vein Patency: A Comparison to Conventional and CO2 Venogram
- Affiliations
-
- 1Department of Radiology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea. chungmic@korea.ac.kr
- KMID: 1443494
- DOI: http://doi.org/10.3348/jksr.2011.65.1.61
Abstract
- PURPOSE
To compare the tourniquet technique (TT) with the conventional venogram (CV) and the carbon dioxide venogram (CO2V) for the evaluation of central vein patency of the upper extremity.
MATERIALS AND METHODS
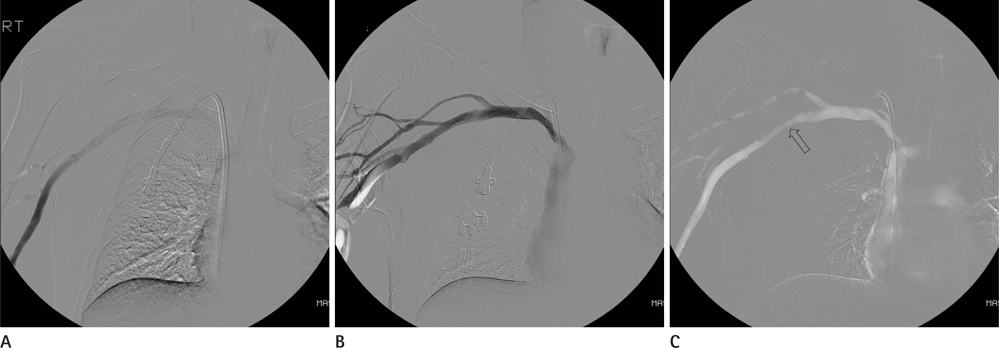
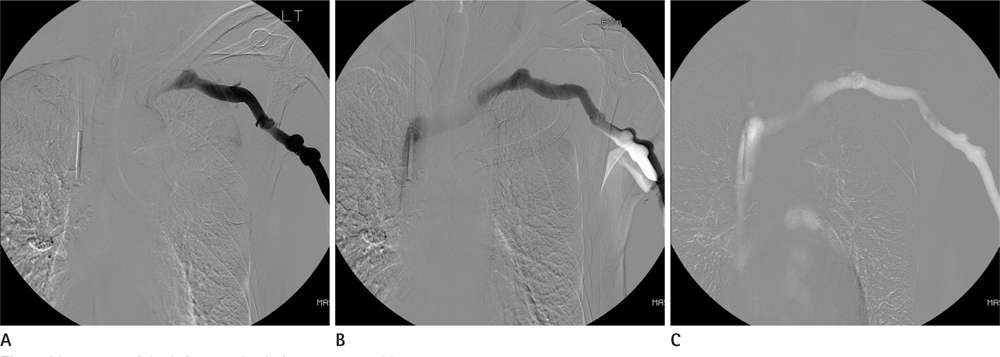
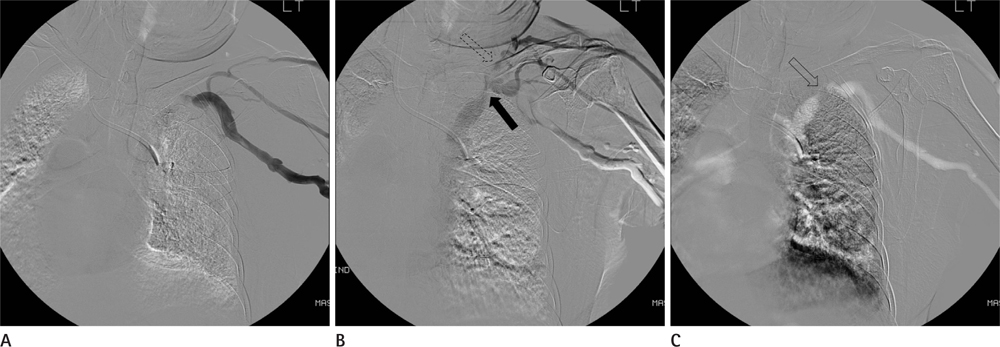
CO2V, TT, and CV were performed on 100 upper extremities prior to an arteriovenous fistula operation. The central vein was divided into four segments. The best image of the venograms for each segment was chosen as a reference, and the venogram techniques for each segment were graded from 1 (invisible) to 5 (excellent) compared with those of the reference image. The grades of the various venogram techniques at each segment of the vein were compared statistically.
RESULTS
For the SVC segment, the mean grades of CO2V, TT, and CV were 4.32, 3.60, and 2.45, respectively. TT is statistically superior to CV but inferior to CO2V. On the brachiocephalic vein, the mean grades of CO2V, TT, and CV were 4.41, 4.37, and 2.77 and were 4.81, 4.85, and 3.78 for the subclavian vein and 4.75, 4.93, and 4.57, respectively, on the axillary vein. On these segments, TT was statistically superior to CV, but no difference was noted with CO2V.
CONCLUSION
TT is superior to CV in every segment of the central vein and presents similar values to those of the CO2V, except for the SVC.
MeSH Terms
Figure
Reference
-
1. Karakayali F, Ekici Y, Görür SK, Arat Z, Boyvat F, Karakayali H, et al. The value of preoperative vascular imaging in the selection and success of hemodialysis access. Ann Vasc Surg. 2007; 21:481–489.2. Chalmers N. The role of vascular radiology in hemodialysis access. Semin Dial. 2002; 15:259–268.3. Robbin ML, Gallichio MH, Deierhoi MH, Young CJ, Weber TM, Allon M. US vascular mapping before hemodialysis access placement. Radiology. 2000; 217:83–88.4. Turmel-Rodrigues L, Bourquelot P, Raynaud A, Beyssen B, Sapoval M. Hemodialysis fistula: preoperative MR venography--a promising but partial view. Radiology. 2000; 214:302–303.5. Heye S, Maleux G, Marchal GJ. Upper-extremity venography: CO2 versus iodinated contrast material. Radiology. 2006; 241:291–297.6. Shaw DR, Kessel DO. The current status of the use of carbon dioxide in diagnostic and interventional angiographic procedures. Cardiovasc Intervent Radiol. 2006; 29:323–331.7. Hahn ST, Pfammatter T, Cho KJ. Carbon dioxide gas as a venous contrast agent to guide upper-arm insertion of central venous catheters. Cardiovasc Intervent Radiol. 1995; 18:146–149.8. Caridi JG, Hawkins IF Jr. CO2 digital subtraction angiography: potential complications and their prevention. J Vasc Interv Radiol. 1997; 8:383–391.9. Kerns SR, Hawkins IF Jr. Carbon dioxide digital subtraction angiography: expanding applications and technical evolution. AJR Am J Roentgenol. 1995; 164:735–741.10. Geoffroy O, Tassart M, Le Blanche AF, Khalil A, Duédal V, Rossert J, et al. Upper extremity digital subtraction venography with gadoterate meglumine before fistula creation for hemodialysis. Kidney Int. 2001; 59:1491–1497.11. Windus DW. Permanent vascular access: a nephrologist's view. Am J Kidney Dis. 1993; 21:457–471.12. Menegazzo D, Laissy JP, Drrbach A, Debray MP, Messin B, Delmas V, et al. Hemodialysis access fistula creation: preoperative assessment with MR venography and comparison with conventional venography. Radiology. 1998; 209:723–728.13. Sullivan KL, Bonn J, Shapiro MJ, Gardiner GA. Venography with carbon dioxide as a contrast agent. Cardiovasc Intervent Radiol. 1995; 18:141–145.14. Hyland K, Cohen RM, Kwak A, Shlansky-Goldberg RD, Soulen MC, Patel AA, et al. Preoperative mapping venography in patients who require hemodialysis access: imaging findings and contribution to management. J Vasc Interv Radiol. 2008; 19:1027–1033.15. Moresco KP, Patel N, Johnson MS, Trobridge D, Bergan KA, Lalka SG. Accuracy of CO2 angiography in vessel diameter assessment: a comparative study of CO2 versus iodinated contrast material in an aortoiliac flow model. J Vasc Interv Radiol. 2000; 11:437–444.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Significance of Preoperative Venogram in Arterio-Venous Shunt Operation
- Deep Vein Thrombosis after Joint Arthroplasty in Lower Extremity: Venography versus Color Doppler Ultrasonography
- Clinical Study of the Changes in Arterial Blood Gas and End Tidal CO2 after Release of Tourniquet
- A Case of Upper Extremity Deep Vein Thrombosis and Pulmonary Thromboembolism in a Severely Obese Man
- A Case of Left Brachiocephalic Vein Total Occlusion Due to Acute Thrombosis Soon after Permanent Pacemaker Insertion