J Korean Fract Soc.
2013 Jan;26(1):69-72. 10.12671/jkfs.2013.26.1.69.
A Case of Surgically Treated by Transperitoneal Approach in Delayed Neurological Deficit after Sacral Fracture: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, KEPCO Medical Foundation, Seoul, Korea. dubalseoki@gmail.com
- KMID: 1431721
- DOI: http://doi.org/10.12671/jkfs.2013.26.1.69
Abstract
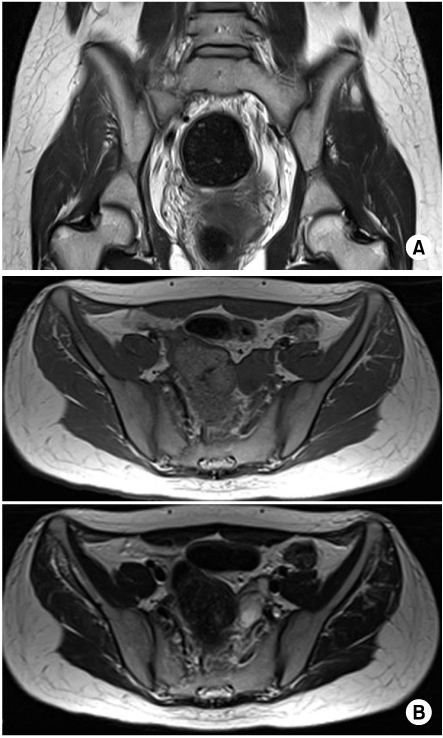
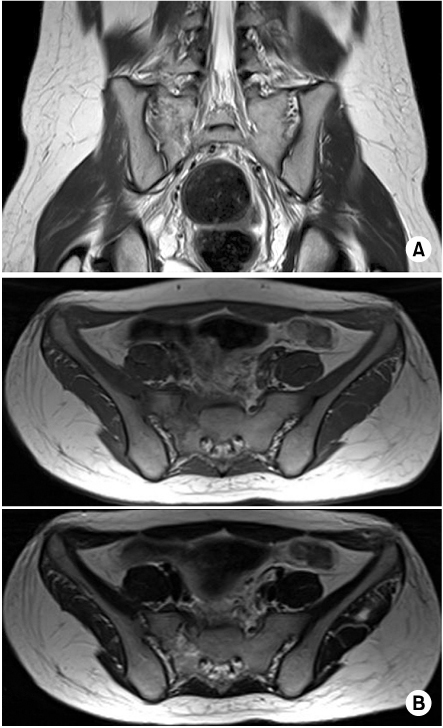
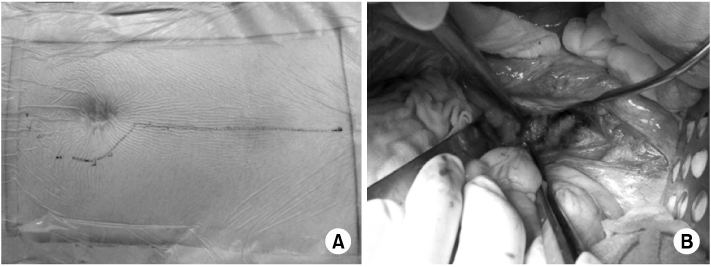
- This study reviews a case of sacral fracture with delayed onset neurological deficit that showed good results after decompressive surgery. The delayed neurological deficit appeared at 4 weeks after injury and it was treated with anterior decompression through transperitoneal approach. A 23-year-old woman was injured in a car accident and had bilateral pubic rami fractures and fractures of the sacral ala on the right side. She was treated with external fixation devices for approximately four weeks, but complained of pain and numbness. The dorsiflexion and plantalflexion of the right ankle was weakened and graded as grade 2. Preoperative pelvic and sacral radiographs, computed tomography, magnetic resonance imaging and electromyelography, and nerve conduction study were performed to identify the region of neurological deficit, and we decided to implement neurological decompression. By transperitoneal approach, we performed bone curratage and decompression around the region of sacral alar slope and S1 foramen. The pain and numbness of the right foot cleared up. Dorsiflexion and plantalflexion of the right ankle improved to grade 5. Anterior decompression by transperitoneal approach proved to bring satisfactory results in a patient, who presented delayed neurological deficit after sacral fracture.
Keyword
MeSH Terms
Figure
Reference
-
1. Bodkin PA, Choksey MS. Management of a sacral fracture with neurological injury. J Orthop Sci. 2006. 11:524–528.
Article2. Chan FL, Chow SP. Retroperitoneal fibrosis after anterior spinal fusion. Clin Radiol. 1983. 34:331–335.
Article3. Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988. 227:67–81.4. Gumbs AA, Bloom ND, Bitan FD, Hanan SH. Open anterior approaches for lumbar spine procedures. Am J Surg. 2007. 194:98–102.
Article5. Kim NH, Moon SJ. The classification and treatment of sacral fractures. J Korean Orthop Assoc. 1992. 27:753–762.
Article6. Lee JH, Kim JU, Jang JS, Lee SH. Delayed neurological insufficiency caused by transverse sacral fracture after minor trauma in elderly patients. Neurol Med Chir (Tokyo). 2011. 51:427–430.
Article7. Papastefanou SL, Stevens K, Mulholland RC. Femoral nerve palsy, An unusual complication of anterior lumbar interbody fusion. Spine (Phila Pa 1976). 1994. 19:2842–2844.8. Patterson FP, Morton KS. Neurologic complications of fractures and dislocations of the pelvis. Surg Gynecol Obstet. 1961. 112:702–706.9. Sasso RC, Kenneth Burkus J, LeHuec JC. Retrograde ejaculation after anterior lumbar interbody fusion: transperitoneal versus retroperitoneal exposure. Spine (Phila Pa 1976). 2003. 28:1023–1026.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Surgically Treated Transverse Sacral Fracture: A Case Report
- The Treatment of Tuberculous Spondylitis of the Lumbosacral Junction by Transperitoneal Approach
- A Case of S1 Radiculopathy in Sacral Insufficiency Fracture without Fracture Line
- Sacral Fracture Dislocation of Suicidal Jumper (Suicidal Jumper's Fracture): 4 Cases Report
- Body Fracture-Dislocation of the Thoracic Spine without Neurological Deficit: A Case Report